Jane’s story
Jane is a 60 year old woman living in Waterloo, Ontario (a number of details of Jane’s case have been changed to protect her confidentiality). For several years she has been experiencing worsening back pain, which was recently diagnosed as spinal osteoarthritis (a degenerative condition that can cause severe back pain). The pain has grown so bad that she can no longer work, and has difficulty moving around her home. Her family doctor wants her to see a number of specialists, including a rheumatologist and spine surgeon. However, the wait to see a rheumatologist in her area is six months, and the wait to see a spinal surgeon is nearly a year. Jane’s family doctor is doing his best to manage her pain while she waits to see these specialists, but it has gotten so bad that only opioid painkillers seem to be effective, and he worries about the risks of using these medications for so long. Both Jane and her doctor wonder why she has to wait so long to see a specialist.
An incomplete picture
Despite almost a decade-long focus on wait times, Ontarians still don’t know how long they are waiting to see specialists.
Canada’s premiers committed to reducing wait times as part of the 2004 health accords, which spawned programs like Ontario’s Wait Times Strategy and the National Wait Times Initiative. Since 2003, Ontario has spent approximately $1.7 billion to reduce wait times for priority areas, including cancer surgery, cataract surgery, hip and knee replacement, and diagnostic imaging. Wait times have decreased in these areas and Ontario now has good wait times by Canadian standards, although not by by international standards. All provinces now monitor and publicly report wait times. Ontario publishes wait times for surgery and diagnostic imaging on the Ministry of Health and Long Term Care’s website.
However, the wait time data published in Ontario represents only the wait between a specialist’s treatment recommendation and a medical procedure such as an operation.
But before a specialist makes a recommendation, there is another wait time – the wait to see a specialist. According to Jon Irish, the Interim Provincial Clinical Lead for Access to Services and Wait Times for the Province of Ontario, the wait to see a specialist can be much longer than the wait between a treatment recommendation and a medical procedure.
While Ontario has made significant progress in measuring and reporting wait times for treatments, there are currently no mechanisms in place to measure or report on the length of wait times to see specialists at the provincial level.
How long are Ontarians waiting to see specialists?
There have been past attempts to measure waits to see specialists, but these have relied on patient or physician estimates, and are widely viewed as unreliable due to low response rates and sample bias. Despite the methodological problems with these studies, there is general agreement that the wait times to see certain specialists can be very long.
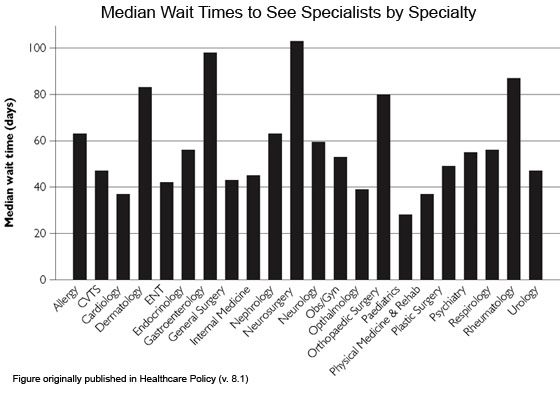
Recent research from the University of Western Ontario supports this view. According to this study, median wait times to see doctors in several specialties in the London area are longer than 80 days. The longest waits were to see a neurosurgeon, a gastroenterologist, a rheumatologist or a dermatologist. Only cardiologists, ophthalmologists, pediatricians and physiatrists had median waits of less than 40 days.
Long waits to see specialists raise the question of why, after such large investments in reducing wait times for treatment, there are no established provincial mechanisms in place to measure, report, and ultimately shorten wait times to see specialists.
This is in contrast to the United Kingdom’s National Health Service (NHS), which tracks wait times from the moment a patient is referred by their family doctor to the time when the patient receives medical treatment from a specialist. The NHS stipulates that 90-95% of patients should wait no longer than 18 weeks (126 days) from the time at which they are referred to the time when they are treated.
Measuring the wait to see a specialist
While the Ontario Ministry of Health and Long-Term Care does not currently monitor wait times to see specialists, an electronic referral tracking system for hip and knee replacements used throughout the Toronto Central LHIN may provide a model for how such a system could work. In 2005, patients being assessed for hip and knee replacement at Sunnybrook Health Sciences Centre were experiencing long waits to see specialists, and staff members had no way to check on the status of referrals.
In response, Sunnybrook introduced a centralized electronic referral system, which allowed staff to monitor wait times to see orthopedic surgeons.
When the Toronto Central LHIN introduced a new model of care for hip and knee surgery in 2007, it adopted Sunnybrook’s referral tracking system and extended it to all six of its hospitals.
The data collected by the referral tracking system is analyzed by Access to Care (a division of Cancer Care Ontario that is responsible for monitoring wait times for all surgery and diagnostic imaging in Ontario), which provides monthly and quarterly reports to the Holland Orthopaedic and Arthiric Centre, which acts as the central intake hub for hip and knee surgery for the Toronto Central LHIN.
According to Lucy Pereira, a program manager at the Holland Centre, data on wait times to see specialists has allowed the Holland Centre to improve their processes, leading to shorter waits for patients. For example, when reviewing the data they observed that their practice of sending a patient’s appointment dates to his or her family doctor was leading to confused patients and missed appointments. “Once we looked at the data, we saw that we should be contacting patients directly with their appointment date, which also gave us the chance to explain to them directly what to expect from their appointment,” says Pereira. Shortening the lines of communication has resulted in better informed patients and fewer missed appointments, which Pereira says has reduced wait times.
The challenge of measuring wait times to see specialists
“Measuring waits for specialists is more complicated than measuring waits for treatment,” says Irish. This is partly due to the sheer volume of patients waiting to see specialists. Irish explains that “only a certain percentage of patients who see a specialist are going on to have treatment, so the number of patients that are logged onto a ‘wait for treatment’ registry will be much smaller than those logged onto a ‘wait to see specialist’ registry.”
In addition, measuring the wait to see a specialist does not always tell the whole wait times story, because referals need to be processed and a specialist may require additional testing before making a treatment decision. Effective measurement of wait times needs to be able to capture both the wait to see a specialist and the wait between seeing a specialist and a treatment recommendation.
Monitoring and reporting of wait times for specialists must also be sensitive to the urgency of patients’ conditions. Patients with very urgent conditions must be seen more quickly, so their wait times must be tracked seperately, as is currently done with wait times for cancer treatment and cardiac surgery.
It can also be a challenge to standardize reporting. Record keeping often varies between specialists’ offices, so data from one office may not be comparable to data from another.
Monitoring waits to see specialists also comes with financial costs. Maintaining databases and performing large scale analysis costs money, and responsibility for reporting these wait times will add to the workload of specialists’ office staff.
Moving towards public reporting
After nearly a decade of investment in shortening wait times for treatment, plans finally appear to be in the works to begin publicly reporting wait times to see specialists in Ontario. Using the systems piloted by the Toronto Central LHIN’s hip and knee service, Access to Care is preparing to monitor wait times to see surgeons across the province, and will publicly report these wait times on the provincial wait time website.
“Access to Care is using a very similar process to what we used for wait times for treatment: first, we establish the process, second we collect the data, third we share the data internally to work through the data quality issues, and then we’ll be ready to report the data publicly,” says Irish.
However, neither Access to Care nor the Ministry of Health and Long Term Care have announced when public reporting of the wait times to see specialists will begin, nor whether the monitoring process will eventually be extended to include all specialists.



The comments section is closed.
I am a 59 year old woman with fibromyalgia, spinal stenosis and biliary dyskinesia. Four years ago I started having gallbladder attacks. Was referred to two surgeons who refused to take out my gallbladder even though my Hida scan ejection fraction was at 4% ( indicates my gallbladder is barely working, spinster of Odi?). Flashforward four years later, lost forty pounds, still in pain, eating severely restricted diet ( only fruit and vegetables) have tried every kind of alternative therapy , acupuncture, laser therapy, meditation etc and still have gallbladder attacks and more severe pain. Am now waiting for a referral to a gastroenterologist and am told it will be a year. Latest blood work shows my bilirubin is up, i can’t keep food down and am severely nauseous and undernourished however this is still not considered serious. I am at my wits end. Any one with any ideas of how to proceed ?
I was getting poor treatment with cortisone shots. Asked my DR. For a referral to another. Now I have 6 to 8 months wait time. I’ll be in a wheelchair bring then. I’m bone on bone in my knee and a 2 yr. Wait for the replacement surgery. I’mean 65 & a post polio person. Depressing. L. Stokes Mar. 11 2017
When travelling, Americans ask about our health care in Canada. I am ashamed of our health care in Canada. It is getting worse and the Ministry of Health is aware. Seems they only do something about it when it becomes critical. True many tests and procedures are free, but the wait times are unrealistic. Given we do not have a two tier health care system in Canada, our health is being jeopardized. The system is broken and needs an immediate fix both federally and provincially. We should not have to go to the US, Europe to get our procedures done, or wait many months or years from reading some of the previous comments I’ve read. We are not a 3rd world country, but heading that way in health care. Those who could afford quick procedures, the funding could go back into the system for those who can’t. It would lessen up the wait times for diagnostic tests, referrals, operations. If people are concerned that those who can afford care upfront, it would mean the rest of us would not have the best doctors, the government could adopt a system whereby doctors would be required to take on a percentage of patients who cannot afford their services. At least lets get medical help a lot sooner. It is useless to have the system we have now free if it involves such long waits. If it is serious such as cancer, heart disease or awful pain to endure and months have to go by, how can we boast about having such a great health care system. It is an embarrassment and ethically wrong.
My husband and I are currently waiting for appointments to see a rheumatologist for fibromyalgia, a pain clinic appointment for chronic post thorocotomy pain, a gastroentologist for chronic pancreatitis, and a vascular surgeon for sever vericose veins The vascular surgeon wait has so far been six months from the time of referral (all diagnostic requirements have already been met). And both appointments for chronic pain where referred 10 months ago. And lastly the referral wait time for the GI specialist is 160 days! You can’t tell me the wait times are as high as 80 days when I’ve been waiting 300 days and counting! And yes the referrals have been followed up quarterly to inquire about progress.
Your article is great. But you must look into the problem of physician gatekeeping. Restricted access to all kinds of medical care is actually an overt provincial policy and a general trend throughout Canada. This affects certain patient populations more than others, chronic care, the elderly and terminal care patients.
I will be frank with you, gatekeeping is the reason many patients are afraid of ‘aid in dying’ because patients are steered away active care programs, and as they decline without care, they will be offered assisted suicide. If you don’t believe this can happen, I’ll send you some research and policy links. In fact, a friend of mine was in palliative care but he was told he could only stay 4 weeks on the unit, that is their maximum stay…even though he only had 6 weeks to live. How is that scenario for setting up a patient for assisted suicide? You have three choices, you can die naturally in 4 weeks, you can be discharged who knows where, or they can offer you ‘aid in dying’. This is all part of gatekeeping, restricting certain patient groups from remedial treatment throughout all stages of a degenerative illness, even palliative care.
In May my doctor submitted a referral to a surgeon I am already seeing for my osto arthritis in my shoulder and was able to get me an appointment or July 12th. That was the good news. My surgeon determined that I need both knees replaced. The earliest possible date is one year for the first knee and six months later he will do the second. In the meantime I will have cortisone injections. This injection takes about 30 seconds but the earliest date is mid September. People should be told that if they feel they may ever get/have arthritis in their their old age and may need surgery perhaps they should try to book a consultation now.
Ontario’s posted average wait times are not worth the key strokes used to post them. My father who is 72 and still working has been diagnosed as requiring a new hip by two doctors. The posted average wait time in Toronto is 4.5 months. My father has been informed that it will be at least 52 weeks before he can meet the orthopaedic surgeon. At this point maybe the 4.5 month timeframe average may kick in. This is what happens when there is a total disconnect between supply and demand in the health care industry. So my father is now looking at surgery in the US where they can look after him in 3 weeks.
Okay, so here is my story. In November 2013, I went to my eye doctor (a clinic with 6 doctors – half of which are ophthalmologists). I had blurry vision in one eye, thinking it was just time for a new prescription (early to mid 40’s). After many tests, one which I had to pay $80 for, I was told it was a retinal problem, and my new glasses did not correct this, so blurry vision in the right eye. On year later, I pushed them to correct this issue, and so another doctor took a look, and I was told I have a cataract. At my follow up six months later, I was told it needs to be treated. So, I had an appointment three months later, and then this specialist recommended I see another one (both at Sunnybrook), so now, July 2015 turns to December 2015. I saw this ophthalmologist, and now, my surgery will be August 2016, which will have been three years that I have put up with having clear vision in only one eye. The fact that this was misdiagnosed in the first place, whereby I lost one year time, should have me getting a push for higher priority, but no such luck. This really has a negative impact on my life, and I cannot wait for the day when I can get my normal life back. Despite what many Canadians, and Ontarians, think, we have a very terrible health care system, as I am sure I am not the only one having to wait this long. Seriously…should this really take this long??? I read that the Ontario Liberals made cuts to cataract surgery, and I cannot wait for them to be tossed out of government, and hopefully, not returned for a very long time. Liberals are the worst governing party, and this is not the first health care change they have done regarding eyes, that has a huge negative impact on people.
Doctors seem too be pushing unnecessary hip replacement surgery. I know it’s a money maker for hospitals. Is this too make the Wynn government look good?
My husband has been in a wheelchair four months..after Mir he was told he has been referred to a neurosurgeon but as reading these comments he probably is looking to at least spring before he sees anyone and then who knows what..is this not I humane? How do we get our government to start addressing this situation and maybe put a law in with a thirty day or else we’ll pay for you to go outside of the country for help
My husband has been diagnosed with Spinal Cervical Stenosis, he is 74 years old and his fingers are all becoming numb, as the spine in C5 and C6 are collapsing and shutting off the nerves, we saw a Neurologist and need to see a specialist in spine problems at a hospital in Toronto, but we can’t even get an appointment and they tell us it will be at least 8 months, by that time he will not be able to use either of his hands, and his pain is unbearable, hopefully he can get into a Pain Clinic, but that also takes time. I have been told that people who are referred to this specialist, like 80% of them can’t be helped by him, why do they not look at the referrals and make a decision as to what patients appear to need to be seen more quickly, much like an Emergency Dept decides which patient is more in need of help at that particular time. Would this not help to stop unnecessary visits from patients who don’t need to see that particular specialist?
NHS states one should wait no longer than 18 weeks. What a joke that is. My family Dr sent a referral to LHSC in June of 2014 to Spine clinic . It took until the end Nov 2014 to receive a letter telling me I had a appointment for March of 2016. If I let my pet suffer like the health care system here in Canada does there sure would be hell to pay.
Today is March 14, 2015 I have a appointment for March 7, 2016 to see a neurosurgeon at LHSC in London Ont. And this is just for a surgery consult. My family doctor told me I was doing well to get in that soon. Our health care system is in the toilet. We can get into big trouble if we let a animal suffer but trying to get a human being looked after is another story. It really frustrates to know that so may OR’s are sitting in darkness while the people at the top are making top dollars to run these places. If I ever won the lottery I would search else where for spine care.
Sorry to hear of your plight…I hope that everything turns out well for you.
Most people are staunch defenders of a public only system. That is…until they get on a waiting list. Until that time, they have no clue how bad it really is.
The government will only pay for so much over time. The result is rationing of care and ballooning wait lists. The need for more service is obvious while operating rooms are open routinely during business hours (except for emergent call in some cases) and surgeons are under and unemployed.
Sheesh…everyone should know what you are going through.
Living in Ontario, Canada is not very promising when spinal surgery is the focus and innovative surgical measures, devices and implants seem rather futuristic and simply non existent. I waited 16 months to see an Orthopaedic Spinal Surgeon. During the consult I was only allowed to address one spinal segment. As a result posterior spinal fusion from T3 to L1 by means of instrumentation rods was recommended with a possible osteotomy. Having cervical and extensive lumbar spine compromise would leave me in a worse physical state if I were to follow through with the proposed surgery.
Nevertheless I have already waited an additional 15 months on a surgical waiting list for a surgery that will probably never come to terms. Living in a country that prohibits private measures to medical care forces patients like myself looking for answers abroad. I have sent my diagnostic imaging to numerous surgical institutes around the world for their surgical opinion and I have had the pleasure of speaking with a number of caring spinal surgeons. The overwhelming recommendation has been addressing the C5-6 and L3-4,
L4-5 and L5-S1 levels with ADR. Of course this surgical procedure is not available in Ontario or throughout the country. In fact, endoscopic spinal surgery is at its infancy here while nations like Korea have been practicing this procedure for over thirty years now. Replacing surgical intervention with narcotics and being slapped with unfounded labels seems to be the answer to more complex spinal situations here in Canada.
Being an Ontarian most of my life I believe that medical treatment is a quintessential right not a privilege. Yet patients are often humiliated and degraded in their journey for help. I say this without prejudice it has been my experience. Most recently I had a chronic pain assessment at the Wasser Pain Clinic in Toronto and sure enough that is what I was labelled with, “chronic pain”. What was really troubling to me was that the doctor was unaware of the surgical proposal that I received and yet without ever looking at my diagnostic reports he concluded that I had chronic pain. He went on to tell me that 1 out of 1000 spine patients actually get surgery for their compromise. It’s a horrible weeding process. Not because a patient does not qualify for surgery, simply, innovative spinal surgical measures are lacking here in Canada. That statement is supported by the Orthopaedic Surgeon from Toronto Western Hospital that recommended my spinal surgery. Going back to my original consult…I was allowed only to address the segment that hurt me the most. When my wife asked if there was anything else that could be done he replied “ unfortunately we still perform spinal surgery in a very archaic way here in Canada”.
I have provided my cervical, thoracic and lumbar spine diagnostic reports. By the way these are condensed second opinion reports that were performed after extensive under reporting from Northumberland Hills Hospital.
LAVERITA
CERVICAL SPINE SECOND OPINION
CONDENSED REPORTS
MRI AND X-RAY
There is straightening of the spine with loss of normal cervical lordosis seen due to paravertebral muscle spasm. There is evidence of grade one retrololisthesis of C2 over C3 and minor retrololisthesis of C5 over C6. Multilevel dehydration and desiccation is seen. The nuchal ligament is hypertrophic at the C6 and C7 levels.
At C2-C3 level, minimal bulging indents the ventral thecal sac. Canal and foramen remain patent.
At C3-C4 level, central shallow herniated disc measuring 5mm in transverse and 2.5mm in AP dimension, indents the ventral thecal sac. There is a superimposed bulge with annular laxity with bilateral uncovertebral joint hypertrophy, this is marginally worse on the left side resulting in mild left foraminal stenosis.
At C4-C5 level, central herniated disc measuring 7mm in transverse and 2.5mm in AP dimension, indents the ventral thecal sac. There is a superimposed bulge. Canal and foramen remain patent. There is bilateral uncovertebral joint hypertrophy.
At C5-C6 level, there is a large herniated disc / osteophyte noted, measuring 12mm in transverse and 3mm in AP dimension in contact with the spinal cord. There is mild canal stenosis (AP dimension is 9.5mm). There is some lateralization to the left side and likely in contact with the left exiting C6 nerve root. There is mild to moderate narrowing of the left lateral recess consequent compression of the left descending C7 nerve root can be expected. Bilateral uncovertebral joint hypertrophy is present.
At C6-C7 level, a disc bulge is seen indenting the ventral thecal sac. Canal and foramen remain patent. The nuchal ligament at the C6 and C7 vertebral level is hypertrophic.
At C7-T1 level, there is no bulge or herniation. Canal and foramen remain patent. There is a small 3.5mm per neural cyst seen in relation to the exiting right C8 nerve.
LAVERITA
THORACIC SPINE SECOND OPINION
CONDENSED REPORTS
MRI AND X-RAY
The vertebral bodies from T6 to T11 show elongation of the antero-posterior dimension. Note is made of mild compression fracture deformities of T7 and T8 vertebral bodies. Schmorl’s Nodes are seen at multiple thoracic levels including T6-T7, T7-T8, T8-T9, T9-T10, T10-T11 and T11-T12 levels representing endplate micro fractures. There is mild disc desiccation seen at the T2-T3, T3-T4, T9-T10 and T10-T11 levels. There is moderate disc desiccation from T4-T5 to T8-T9 levels. Mild reduction of disc height is seen from T6-T7 to T10-T11 levels. Type II modic endplate changes are seen at the T11-T12 level. There is evidence of mild dextroscoliosis at the apex, approximately at the T9-T10 level. There is moderate degree of anterolateral osteophytosis seen worse on the right side caudal to the T3-T4 level.
At T1-T2 level, there is annular disc laxity causing mild left foraminal stenosis. Minimal hypersclerosis is seen with minimal anterior and posterior marginal osteophytosis.
At T2-T3 level, minimal hypersclerosis is seen with minimal anterior and posterior marginal osteophytosis. No canal or foraminal stenosis.
At T3-T4 level, minimal hypersclerosis is seen with minimal anterior and posterior marginal osteophytosis.
No canal or foraminal stenosis.
At T4-T5 level, minimal hypersclerosis is seen with minimal anterior and posterior marginal osteophytosis.
No canal or foraminal stenosis.
At T5-T6 level, minimal disc bulge indents the ventral thecal sac. Canal and foramen remain patent. Mild endplate sclerosis is seen. There is mild facet arthropathy. There is mild to moderate anterior and posterior marginal osteophytosis.
At T6-T7 level, minimal disc bulge indents the ventral thecal sac. Canal and foramen remain patent. There is moderate endplate sclerosis. There is mild facet arthropathy. There is mild moderate anterior and posterior marginal osteophytosis. There is mild costo-transverse joint arthropathy seen.
AT T7-T8 level, minimal disc bulge indents the ventral thecal sac. Canal and foramen remain patent. There is moderate endplate sclerosis. There is mild facet arthropathy. There is moderate anterior and posterior marginal osteophytosis. There is mild costo-transverse joint arthropathy seen.
At T8-T9 level, central herniated disc noted measuring 6mm in transverse and 2.5mm in AP dimension producing mass effect on the spinal cord and demonstrates spinal cord flattening and borderline canal stenosis. Mild loss of joint disc space is seen. There is moderate endplate sclerosis. There is moderate anterior and posterior marginal osteophytosis. There is mild facet arthropathy. There is mild costo-transverse joint arthropathy seen.
At T9-T10 level, minimal disc bulge indents the ventral thecal sac. Canal and foramen remain patent. There is moderate endplate sclerosis. There is mild facet arthropathy. There is moderate anterior and posterior marginal osteophytosis. There is mild facet arthropathy. There is mild costo-transverse joint arthropathy seen.
At T10-T11 level, There is moderate endplate sclerosis. There is mild to moderate anterior and posterior marginal osteophytosis. There is mild facet arthropathy. There is mild costo-transverse joint arthropathy seen.
At T11-T12 level, shallow herniated disc indents the ventral thecal sac. There is moderate endplate sclerosis. There is mild to moderate facet arthropathy seen causing mild to moderate right and mild left foraminal stenosis with the disc / osteophyte seen in contact with the exiting right T11 nerve root.
OTHER DIAGNOSIS IN PART OF THE THORACIC SPINE
1) SCHEUERMANN’S DISEASE
2) DISH (DIFFUSE IDIOPATHIC SKELETAL HYPEROSTOSIS)
LAVERITA
LUMBAR SPINE SECOND OPINION
CONDENSED REPORTS
MRI AND X-RAY
There is disc desiccation from L2-L3 to L5-S1. Mild reduction of disc height is seen from L2-L3 to L5-S1, most marked at the L5-S1 level. Shallow schmorl’s nodes are noted from L2-L3 to L5-S1 levels. Dextroscoliosis is noted with the apex at approximately at the L4-L5 level. Note is made of minimal grade one retrololisthesis of L1 over L2. Grade one retrololisthesis of L2 over L3 is not appreciated measuring 4mm. There is grade one retrololisthesis of L4 over L5. Multi-level spondylolisthesis with evidence of ligament instability. Mild degenerative changes at both sacroiliac joints. Note is made of L5 segments sacralised to the ala of the sacrum.
At the L2-L3 level, there is an annular disc bulge seen. There is a superimposed far right paracentral herniated disc with associated annular tear. There is mild to moderate right and mild left foraminal stenosis with disc / osteophyte seen in contact with the exiting right L2 nerve. Canal is patent. Moderate endplate sclerosis is present. There is mild to moderate facet arthropathy / ligament flavum hypertrophy noted. There is moderate anterior and posterior marginal osteophytosis in conjunction with spondylolisthesis and spurring.
At L3-L4 level, bilobed annular disc bulge is seen with bilateral intraforamen extension. There is a shallow left and right parietal disc herniation present. There is mild to moderate foraminal stenosis with disc / osteophyte seen in contact with both exiting L3 nerves. There is no canal stenosis but the disc is also in contact with both descending L4 nerves. There is mild to moderate endplate sclerosis present. There is moderate anterior and posterior marginal osteophytosis. There is moderate facet arthropathy / ligament flavum hypertrophy seen.
At L4-L5 level, annular tear is visible. There is a central herniated disc measuring 10mm in transverse and 2.5 mm in AP dimension that indents the ventral thecal sac. The canal is patent. There is a superimposed bulge with bilateral foraminal stenosis and mild left lateral stenosis. Corresponding compression of the bilateral L4 exiting nerve can be expected. There is mild endplate sclerosis with minimal anterior and posterior marginal osteophytosis. There is moderate facet arthropathy / ligament flavum hypertrophy.
At L5-S1 level, diffuse disc bulge is noted. There is a superimposed left paracentral disc / osteophyte herniation noted. There is mild to moderate bilateral foraminal stenosis and left lateral recess stenosis. Corresponding compression of the bilateral exiting L5 nerve and left traversing S1 nerve can be expected. The canal is patent. Mild endplate sclerosis is noted. There is mild to moderate facet arthropathy / ligament flavum hypertrophy.
OTHER DIAGNOSIS IN PART
OF THE
LUMBAR SPINE
1) BILATERAL SACRALIZATION OF THE TRANSVERSE PROCESS
2) SPINA BIFIDA OCCULTA
3) DYSPLASTIC (FALSE ORIENTATION) OF THE RIGHT SUPERIOR ARTICULAR PROCESS
OF THE SACRUM
4) BILATERAL SACROILIAC DISEASE
5) OSTEOCHONDROSIS OF THE FACETS AND SPINOUS PROCESS
The original thoracic spine MRI conducted at the Northumberland Hills Hospital concluded two minor disc bulges that appear non compressive. Sure, medical deception is amongst us. Not that it’s a lie. The truth is, it’s an opinion. A report is the bases of why a patient is placed on a wait list to see a specialist or surgeon and yet for what ever reason this actually happens. Is it because a radiologist lacks the competence, or…
To this end a patient’s care goes way beyond the struggle of wait times. I can attest not only because of my experience with my extensive spinal damage but the heart attack that could have been avoided if it were not because of the negligence of my past G.P. The gate keeper to our health and wellness does lie in the hands of our general practioner and it usually reflects why patients wait so long for the appropriate help. After my G.P realized that my spine was a “train wreck” he would not even facilitate physiotherapy for me. He told me the best therapy would be a hot tub. As far as a referral I was told the only way I was going to see a surgeon was if I had a way in…He did however recommend that I could go to India to a white persons hospital or perhaps contact the Toronto Argonauts Medical Team and they might see me in their off season…It goes on and on. I am not complaining, these are merely my experiences. There has to be a complete reform on how medicine and treatment is conducted in our country. My stand point in this statement is that I have paid income tax since the age of 16 and our medical system should not be viewed as a privilege, it’s our right.
LAVERITA
I’ve gone live with my story, should be published in the London Free Press during week ending October 23, 2016
I have been in severe sciatic nerve pain for 10 years. No drug can alleviate the pain. I wake up to pain and go to bed with pain. Sometimes it’s tolerable, sometimes not. I spent 3 days this week in bed trying not to move it and not putting any wait on it. The drugs are for making me “stoned” because the pain is beyond tolerable, beyond 10 out of 10. If I didn’t use drugs during those times I would loose my mind. I have seen 5 Ontario surgeons who said the identical words. “I can’t see anything” after viewing my MRi. So I went to Florida and had 3 surgeries. Same pain still. Their answer,” You just need more surgery, give us more money.”
I ran out of money. So now I am in the same horrific pain. Unable to work. I receive $ 348. per month disability pension. And no savings left. But . . . I keep meeting people that tell me they had the same symptoms and were able to get the necessary surgery, right here in Ontario. The youngest being 23 and the oldest being 80 and every age in between. But not for me ? I do not live. It’s merely a long and painful, protracted death. When it’s bad, I lay in bed and beg God to kill me or swear at the TV or thin air. Or sometimes just lay there and cry. This happened when I was 45 years old. What a shameful waste of a life. I could have done so much. Alan.
Ministry of Health website underestimates cataract wait by 1/2 as 2nd eye not considered “on wait list” until 1st eye is done.
Just to add, if/when we start capturing the next level of wait times (i.e. family doc to specialist), we should be capturing the time to see the next available specialist, not to a specific specialist.
Patients would then able to get to decide if they want expediency or wait for a specific specialist. Moreover, from a queueing theory perspective, one centralized list is more efficient and most fair for the entire system.
There was an example in the news recently about a patient having to go to Turks & Caicos to get a knee replacement done, but I wonder if there was another capable surgeon with OR time somewhere else in the province who could’ve done it.
Link to article: http://www.calgaryherald.com/health/Have+scalpal+will+travel+Alberta+surgeons+operate+abroad+bypass+wait+times/9405898/story.html
Brilliant article – Thanks so much for writing it!
%featured%While reporting isn’t perfect, I’m so thankful it’s being tried. Pay4Results has transformed senior administrators’ interest in emergency department operations. Things that get measured get fixed.%featured%
Again, great topic; well done!
Shawn
http://www.stoppatientwaiting.com
The Canadian Association of Gastroenterology has been capturing wait times for several years now; both the time from primary care physician to specialist and the time to specialist consultation or procedure. This work has been reported and can be found at
http://www.cag-acg.org/special-projects/wait-times
and at
http://www.cag-acg.org/component/content/article/1-latest-news/1716-cag-releases-2012-sage-wait-time-data
Excellent article. At the inception of the Ontario wait time project we had to decide on the project scope within the fiscal and time constraints imposed by the Government. The intention was that additional wait time measurements would be added to the package, once a province wide program of data capture, analysis and reporting was a reality. Its time to add to the great success of the initial program which was accomplished by hundreds of dedicated individuals across Ontario, lead by Sarah Kramer.
%featured%A significant reduction in the wait to see a specialist can be accomplished by ensuring that only appropriate cases are on that waiting list.%featured% Not every headache patient needs to see a Neurosurgeon. Jim Waddell has lead an excellent process of setting up a simple triage algorithm so that only appropriate hip pain patients are seen by Orthopaedic surgeons. The care provider is frequently not a surgeon. All specialities should follow the lead of the Orthopods in communicating simple threshold rules which will prevent wasting the patients and specialists time by inappropriate referral.
I sure do agree with the appropriate cases theory. I know one person and she used up TWO appointment slots only to see the specialist and the refuse any help. This is because she claimed she hurt her back at work when it was from a accident at home. This is so she could get workers comp. Makes you wonder how many more are doing the same.
i was informed that i have a second intraneural tumor in my calf. i had one removed in 2010. the specialists office has told me not to expect to hear from them for an office appt for at least 20 months. i find that ridiculous. we may want to find out if its benign or not before we wait 20 months for this appt.
Reality is that the total wait time should encompass
1. the wait to see the family doctor (sometimes weeks)or other referring professional
PLUS
2. the wait for various diagnostics that the primary care provider might order (weeks or months for ultrasounds, MRI, CT, stress testing etc) before referring to the specialist
PLUS
3. the wait to see the specialist (weeks or months or YEARS)
PLUS
4. the wait to have other diagnostics done via the specialist
PLUS
5. the wait for OR time or other publicly funded infrastructure requirement.
In total, patients can easily wait for 6 months to a year (or longer) for many standard types of care.
With the aging of the population with increased levels of acute and chronic disease we can expect wait times to increase despite more and more public spending.
%featured%Measuring and monitoring are not the fix needed but would help to quantify the extent of the problem. However, tax dollars spent to quantify the problem do not provide the front line care needed.%featured%
I was told by a friend in the health profession that it could take up to 6 months to see a specialist. My family doctor kept insisting that I wait another 6 months,and then another 6 months, to see what was happening..the condition had been there for over a two years. With the information from my friend, I insisted on being referred to a specialist. I still had additional monitoring tests done with the family doctor during the 6 month waiting period which was used as extra documentation for the specialist. If not for the heads up from my friend, I would have been oblivious to the 6 month waiting period to see the specialist and would not have so strongly insisted upon the referral. It is a fact of which everyone needs to be aware.
Thank you. An excellent and important article.
I have a family member who is in the position of waiting for a call from the surgeon after a radiologist reported a risk of cancer and the family doctor made a referral. Anxiety is growing as the wait continues. I finally called and was told that they way it works is that the referral to the surgeon is then sent to a central location that evaluates and prioritizes patients. Once that is done, the surgeon’s office will call the patient. I asked, “and how many months will it take after that?” I was told that the surgeon would see the patient within a month of the call.
From your article, I now understand that the reported wait times would be less than one month. I would like to add that I believe that the process of prioritization should be made public– both in the manner in which it was developed and the guidelines that exist.
Thanks for asking the good question. It’s obvious that the numbers are not something to brag about, or they would have been published.
The University of Western Ontario estimate of mean wait times for specialists, being over 80 days, is one more bellwether indicator that Ontario’s Health Care System is in a moribund state –and gravely in need of systemic change.
Too much of the money being thrown at the system is going into the pockets of bureaucrats and administrators (i.e. the eHealth scandal), rather than to core health needs.
Sadly, with our aging population bulge, wait times will increase and health services will continue to decline until more resources and attention are focused on disease prevention.
For more on health care sustainability, go to:
http://ophealthchoices.wordpress.com/2012/10/15/vision-of-a-sustainable-health-care-system/