Bill is an elderly patient living independently at home, who recently fell and was admitted to the hospital where I work (name and minor details changed to protect his identity). Bill clearly indicated his wish to spend as much time at home as possible.
For some time we had been measuring our length of stay in hospital, and more recently we had been monitoring our readmission rate. But Bill presented us with a dilemma. On the one hand we could achieve the shortest length of stay by sending Bill directly home from the emergency department, without assessment or home services and with the high likelihood that he would soon be re-admitted. Alternatively, keeping him in hospital indefinitely would eliminate the chance of re-admission. However, optimal care for Bill would produce mediocre scores on both measures. What we did not have was a single measurement that would reflect best care for Bill, and help us to meet his goal of spending as much time as possible at home.
Every industry faces the challenge of simultaneously optimizing both efficiency and quality. Before becoming a doctor, I worked as a manufacturing engineer at a company producing circuit boards. Despite our best efforts during the production process (the “length of stay” at our factory), a small number circuit boards would require repairs before shipping or be returned by customers for repairs (“readmissions”). We therefore measured the cycle time, meaning the total time that a circuit board was in our factory, including during production (length of stay) and for repairs (readmissions). If our average cycle time was low, then we knew that we were manufacturing efficiently and achieving high quality.
I believe that in health care, cycle time – the time that it takes from beginning to end of a treatment process, including if necessary, the treatment of complications – should replace wait time as a key measure of health system performance.
Long waiting times to access health services are a major concern in Canada, and wait times for parts of the treatment process are being monitored. However, if we aren’t measuring the cycle time (the total process time), then it is predictable that efforts to shorten wait times in one area will lead to longer wait times somewhere else. If a surgeon books additional surgeries to clear a backlog, then this is likely to come at the expense of their availability to see new referrals. The result is that patients wait longer for their initial assessment. Imagine a mechanic who advertises same day service, but has a 3-month wait list to get an appointment! And there’s no guarantee that efforts to shorten wait times in one area don’t actually increase cycle time overall.
Because most diseases lead to progressive disability, delays in completing treatment are not just inconvenient, but lead to worse health outcomes and higher costs. Long cycle times are highly undesirable.
There is evidence that shorter cycle times are associated with higher quality and reduced cost, in other industries as well as in healthcare. The concept of cycle time has been applied in outpatient settings, and in hospitals around the world. However, cycle time should be applied more often to the entire journey of patients through our health systems, from referral to discharge.
Efficiency rises when cycle time is short, because care has been provided in less time, using fewer resources. Because cycle time includes the impact of complications, low cycle time also represents high quality. For example, in comparison to measuring length of stay and readmission rates, cycle time is a superior measure of hospital performance and value.
We need a better way to measure health care performance for patients like Bill, his care providers and the taxpayers funding his care. I suggest that we adopt cycle time as a key indicator of health care performance. More widespread efforts to monitor and reduce cycle time are required to ensure high quality, affordable, high value health care.
Cycle time and cost
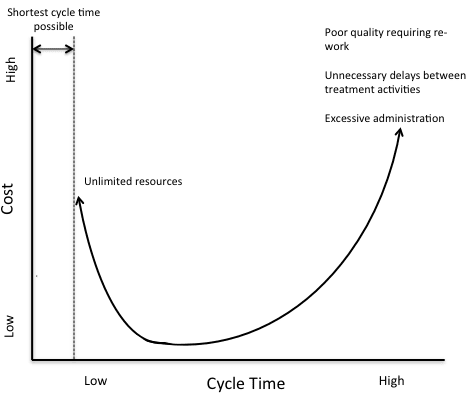
The shortest possible cycle time is defined by the minimum time required to provide all medically necessary services. Although in general shorter cycle times save money, the minimum cycle time can only be achieved if there are no resource limitations, and therefore relatively high costs. The lower left segment of the curve therefore represents the highest value (short cycle time, low cost and high quality).
Nine rules to achieve low cycle time
So what does this mean on the ground? There are several practical rules that, when followed, will shorten cycle times. I believe applying these rules to health care processes can save money and increase quality.
1. Cycle time must include treatment complications.
If we just measured cycle time from referral to discharge there would be incentives to skip treatment steps, discharge people home too early, and just deal with problems later on.
But if cycle time includes the treatment of complications, then it is safe and appropriate to reduce cycle time as much as possible. Cycle time for a surgical process would start at the time of referral and end when the patient is discharged home post-surgery. However, if the patient developed a post-operative complication, the cycle time clock would be re-started during further management.
When treatment complications are included, then short cycle time can only be achieved by providing optimal care.
2. The constraint should be at referral, the first process step.
The constraint (or “bottleneck”) is the slowest step in a process. The constraint therefore determines the rate of the entire process. A wait list will always develop before the constraint.
When the constraint is at the first step, for many health processes this would be referral, then the number of patients being referred and discharged are balanced. Wait times do not grow inside the process, and cycle time is minimized.
A short, stable wait list for referral may be a useful buffer to even-out demand and capacity. However, if the referral wait list increases, then the capacity of the entire process must be increased (rather than just accepting more patients and hoping for the best).
3. Cycle time must be regularly monitored.
If cycle time increases then it is possible that the constraint has shifted to a different step in the process. Wait times at each process step should then be measured to find the new constraint.
Wait times should be measured as patient-days, because either a small number of patients with long waits or a large number with short waits represents a problem.
4. Once the constraint has been identified, that step should be sped up.
Speeding up the constrained process step increases the capacity of the entire process.
After the constrained step is sped up, the constraint will shift to a new step. Constraints within the process should be identified and eliminated one by one (until the constraint moves back to the first step, where it belongs).
5. Process steps should be allowed to idle.
In a treatment process that is constrained at intake, all other steps have extra capacity. Health providers (and/or treatment equipment) will have idle time while waiting for a patient to complete the prior step. This is acceptable, and even desirable. As long as cycle time is not increasing, then idle time is an indicator of efficiency.
6. Process steps should be completed in parallel whenever possible.
Parallel process steps prevent unnecessary waiting for sequential treatment activities and therefore significantly reduce cycle time.
7. Treatment should be as standardised as possible.
At least 80% of patients should progress through a standard treatment process. Time that is gained (through greater efficiency) by treating the majority of patients in a standard process can be used for the minority of patients who require extra, more individualized care.
8. Protocols should be followed for the standard treatment process.
Protocols reduce the variability of the process (and therefore reduce the cycle time). The standard treatment protocol should apply to the 80% of patients that follow the standard process. On the other hand, patients that are not in the standard process should not necessarily be treated according to a protocol.
Adherence to protocols can be improved by adopting a policy of “comply or explain”. Non-compliance that is well explained then provides feedback to improve the protocols.
9. The most expensive process step may justify the creation of a buffer (wait list) to ensure that it is always in use.
The most expensive process step should be maximally utilised. To achieve this, a short buffer (or wait list) may be created to compensate for variations in capacity and demand.
For instance, MRI scanners are expensive and in high demand. A short buffer for MRI can help to ensure that the machine is maximally utilized.
Any buffer should have a clearly defined maximum wait list to ensure that it does not grow unnecessarily long. If this maximum is exceeded, then no additional patients should be accepted into the process until the cause of the delay is identified and fixed
Example: using cycle time in the operating theatre to improve performance
All hospitals have a wait list for the operating theatre. This “buffer” ensures that the operating theatre is not idle if a patient arrives late or is cancelled. Let’s imagine that at a particular hospital the operating theatre is fully booked with knee replacements. The surgical team can complete 4 per day with an on-call wait list of 2 patients. In the operating theatre there is a problem with the cautery machine, which works intermittently. Surgeries proceed because this is not considered a serious issue, but each surgery takes 10 minutes longer. Therefore one patient who is scheduled for a knee replacement is delayed to the following morning. The following day the on-call wait list is now 3 patients, and due to the cautery problem another operation is delayed. By the next day the on-call wait list has grown to 4 patients.
None of the operating room staff report the misbehaving cautery machine, because there are often small problems in the operating theatre and nobody notices the extra time that surgeries take. At the hospital there is no protocol for how big the on-call wait list can be, so the pre-surgical clinics continue to book 4 new patients every day.
Problems cause cycle time to increase
By the end of the 5th day, there are 6 patients in the on-call wait list. The cycle time for the entire process has increased by 4 patient-days, and every day the cycle time increases by one patient-day. Even if the problem is now fixed, an extra day and a half of operating time is required to clear the backlog. If the backlog is not cleared, then cycle time has permanently increased. And we know that longer cycle times cost more money and result in lower quality care. There are only two solutions: either stop booking new patients or temporarily increase the operating theatre capacity (usually by booking longer days or an extra shift).
Monitoring cycle time allows rapid resolution of problems
Now imagine that cycle time is well monitored. Particular attention is given to monitoring the operating theatre on-call wait list, because that is an indicator of problems. A maximum on-call wait list of 4 patients has been defined. Reaching this maximum on the second day triggers the pre-surgical clinic to stop booking new patients for surgery. A rapid-response team is activated to find the problem, and within an hour they have identified and solved the issue (in this case, by replacing the faulty cautery machine). An extra half-day operating session is scheduled to clear the backlog, and the pre-surgical clinics resume.
Monitoring cycle time allowed rapid identification of a problem that may have continued unnoticed. Cycle time, which trended briefly up, is back to its baseline, meaning that costs are well controlled and the quality of patient care is high.


The comments section is closed.
Excellent article. As an industrial engineer with a manufacturing background working as a management consultant in many industries (including ,healthcare), I concur with everything in your article. Once the cycle time is being properly measured we can move on to more advanced techniques based on the distribution of cycle times, including statistical process control (including parrot analysis) and over-capacity scheduling which will, over time, incrementally improve average cycle times and reduce the costs associated with disrupting the normal process, like having to re-schedule procedures.
….does not apply if you perform as a ” knowledge worker” VS. “service worker”
Excellent post.
The Cycle Time seems to go hand-in-hand with care bundling. The major challenge is in involving multi disciplinary teams in taking responsibility and developing governance mechanisms for the cycle of care, not just individual procedures. A promising metric, but not sufficient to effect change.
” inter” ( not multi)….. and each part should be financed per event ( regardless of participation) to ensure continuity for client ( regardless of severity fluctuations).