As a recent ophthalmology and retina surgery graduate, I was shocked by the dramatic unilateral healthcare cuts announced in May. This left me with a poor first impression of the relationship between the health care profession and government. Although the OMA and government are back at the bargaining table, I am concerned that the best interests of the patient may not be represented. It is increasingly frustrating to hear the same myths perpetuated by government officials.
One myth is that the quality of health care services will not be affected. In reality, compromising essential services will threaten patients’ vision and quality of life. One example from my specialty is that payment for optical coherence tomography (OCT) tests is now limited to 4 tests per patient per year. OCT technology allows for high-resolution images of retinal tissue structure – essentially providing a biopsy of the retina without requiring any invasive procedure.
Multiple clinical trials have proven that blindness can be prevented in patients with wet macular degeneration. Some trials suggest that intraocular drug injections, when given monthly, are superior to injections given on an “as needed” basis. However, a more popular approach is a compromise between the two, known as “treat and extend”, which reduces the costs and complications associated with monthly treatment. This requires that OCTs be performed more than 4 times per year. Without doing the OCT, doctors may instead provide injections more often than required. What is the cost of limiting $25 OCT tests? More patients may require injections costing up to $1700 per shot, while also increasing the risk of complications. Penny wise, but pound foolish.
Another myth is that the breadth of services provided in healthcare will not be affected. These cuts de-incentivize technology, so in the future ophthalmologists in Ontario will no longer be able to invest in the most up to date diagnostic equipment. Patients may have to travel outside the province to receive imaging that ophthalmologists have established as the standard of care.
The most pernicious myth is that there were no fee cuts, just freezes. The reality is that some of the most commonly performed ophthalmological procedures and diagnostic tests were cut substantially. For example, compensation for OCT was cut from $63 to $25, which along with the reduction of from 6 tests per year down to 4 amounts to a 74% cut. In June, Ontario retina specialists in an informal survey reported a 34% reduction in income as a result of the cuts – clearly not just a freeze in compensation. Some have self-reported a 50% drop in income since. This comes on the heels of our voluntary offer and implementation of a 16% cut in reimbursement in 2011.
To date, the Ontario government has refused to declare how they came to their decisions on the implementation of these cuts and who was advising them. As a member of the Canadian Retina Society and the Ontario Society of Retina Specialists, this was discussed at our meetings in June and September. Other provincial governments have sought out retinal subspecialists to understand the services they provide in an effort to make well-informed decisions on budgetary amendments. The fact that the Ontario government has not also taken this step has been troubling, considering the solid record we have of working with government to seek out cost savings that are not detrimental to patient care. The profession recognizes the current economic situation and is willing to find ways of reducing public health care spending with the least impact on patient care, but we have not been allowed meaningful input.
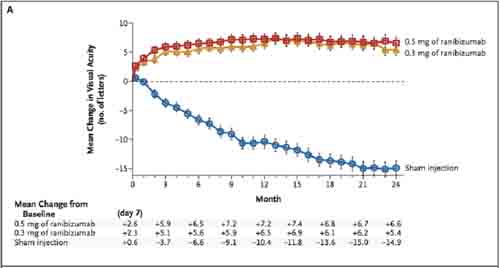
Retina specialists have been fortunate to witness exceptional advances in their field in the last decade. Patients with wet macular degeneration can now be saved from blindness. Intraocular injections of Avastin and Lucentis (see chart below) can dramatically improve vision in 30% of patients and can stabilize the vision of another 60% of the population. This is very different from 2004, where the majority of patients lost vision. Injections also help improve the quality of life for patients with diabetic retinopathy who can more quickly re-enter the workforce. The cost of any of these indicated diagnostic tests or treatments is not even comparable to the cost of social services for a blind patient (e.g., disability payments, transportation, home services, etc.).
Since 1991, the Ontario population has increased by 31%. The number of ophthalmologists has only increased by 8%. The number of procedures performed has increased by 18% since 2006. This has led to fitting in an extra day of work into an ophthalmologist’s schedule. This increase in workload actually stemmed from the request of the government to decrease wait times.
I have only been in practice for two years, but I was drawn to this profession because ophthalmologists are passionate about their work, adapt to ever-changing technology, and are appreciative of the opportunity to provide better healthcare with every passing year. I am extremely grateful to my colleagues and for the privilege to provide retina care in Ontario. But I do fear how our practice will change if the government continues to ignore our clinical recommendations and evidence-based medicine, and deprives patients of the diagnostic and therapeutic technology that makes our specialty so fascinating.


The comments section is closed.
This infighting does nothing to protect the medical profession from the whims of outside interests (corporations, hospitals, governments).
Instead of insinuating that an ophthalmologist gets paid too much, we should be fighting for more attractive pay for our underpaid colleagues like family doctors, psychiatrists and pathologists.
A bunch of self-important narcissistic fools, doctors are.
Dr. Hillson, do you have to pay any office staff out of your OR billings?
Yes, the typical eye surgeon pays about 40% of all billings including OR billings to cover office overhead expenses. By the way, eye surgeons have the highest practice expenses of any medical practitioner according to the 2010 National Physician Survey (Canadian), about 1/3 higher than the next highest group.
5 G for a 7 hr day just a bit better than the payscale for a 16 hour neurosx procedure.
John Smith I think you may find it more useful to address the poor reimbursements for neurosurgeons. Cutting cataract surgery reimbursements down to $50 a case will not make your day of neurosurgery any easier and it will impair patient access to a much needed service.
Actually this comment is incorrect. There is a fixed pool of funds for OHIP billings – 11 billion and as other specialties get more money, other specialties get less. 20% or 2 billion of OHIP funds go to just 8% of physicians primarily in the following specialties – DI, Ophthalmology, GI and Cardiology. So, there is a relationship between high amount of funds allocated to one specialty, say ophthalmology and a lower amount of funds allocated to another specialty, say Neurosurgery
Ophthalmology’s slice of the global budget to MDs has not increased to my knowledge. If anything it has decreased with relativity adjustments. Read the article: ICES data shows us that Ontario’s population has grown 31% in the past 20 years, while the number of ophthalmologists in Ontario has increased only 8%. Cardiothoracic surgeons increased their numbers by 50% over the same time period. The average ophthalmologist provided 20% more services in 2010 than were provided in 2006. As the outnumbered docs struggle to provide service to a growing (and aging) population, we should not be surprised that per MD billings increase for slow growing specialties like ophthalmology
Once again incorrect. The proportion of the surgical physician services budget consumed by ophthalmology has grown from 15.9% to 18%. While the number of ophthalmologists has increased only 8%, this has not been because of a lack of funding for training positions. The Ministry has funded training positions and re-entry training for ophthalmology but the programs themselves have severely limited number of training spots for entrants, while taking increasing international medical graduate positions. One possibility is the specialty controlling supply to keep incomes high. All specialties are “struggling to provide service to a growing and aging population”, not just ophthalmology. As an example, the same ICES data from 1992/93 to 2009/10 shows that the number of Otolaryngologists, or ENT Surgeons, have grown from 239 to 248, or increased only 3.7%, yet their median billings have increased only 33%, from $300,00 to $400,000. However, ophthalmologists have increased much more – 8% – while their median billings have increased from $300,000 to $600,000 or a whopping 100%.!
Hmmm….30 min per surgery!!! one of the cataract surgeons at my hospital books 30 cases in a 8 hr day.
My 30 minutes comment represents average booking times for an average cataract surgeon. I’m sure you know that as 30 minutes is an average, some surgeons will be faster than that and some will be slower. I personally book 15 cases in a 7 hour OR day.
This is a video of modern cataract surgery. It is more intense than years ago because most of the time in the past was taken by the placing of about 10 sutures. This was tedious but the least risky time of the surgery. Now zero to 2 sutures are placed. Also the surgery looks much easier than it really is because the video is in 2 dimensions while the actual surgery is done in 3-dimensions. The depth between the back of the cornea and iris is 3 millimetres. Just touching this wrong place can cause damage that can cause pain and poor vision for the rest of the patient’s life.
http://bit.ly/RJCjc8
You are correct, cataract surgery can be done more quickly today than 30 years ago. Today the average cataract surgeon books one cataract surgery every thirty minutes, versus the 40-60 minutes 30 years ago. What most people don’t realize is that reimbursements for cataract surgery have also dropped. Reimbursements today are less than 50% what they were in 1980, when inflation is factored in. In the past three years alone, reimbursements for cataract surgery in Ontario have been reduced by 25%. As far as the surgery being “easier”, it is safer and more predictable than ever, but the expertise required has also increased. In fact, ophthalmology residencies are one year (25%) longer today than they were in the two decades ago. Patient expectations for excellent results are higher than ever, and outcomes that would have been fine 20 years ago like uncorrected astigmatism are often not accepted today. So yes, the surgery is quicker, but it is in many ways more challenging than ever. And the surgeon reimbursements have dropped significantly already.
I know very little about ophthalmology, but I understood that it has become far easier to perform procedures like cataract surgery because of technological innovations. It is safer and require significantly less time. As a result the fees probably should go down. Am I mistaken?