Cheryl Prescod is not afraid of an uphill battle.
Immigrating to Canada as a child from Guyana started her off at a systemic disadvantage early in life. As a Black woman, she’s familiar with racism and feeling excluded – and continues to see these experiences reflected in her three children as they grow up.
“Social exclusion (can) lead to poor health, especially mental health issues,” she says. “It’s traumatic for many people that look like me.”
Prescod says she decided to become an advocate for marginalized groups about 30 years ago. Initially doing laboratory research, she says she “traded test tubes for people” shortly after participating in community volunteering.
“I thought it was a much more rewarding way of making an impact,” says Prescod. “I know that my academic training helped me to actually think of solutions to problems (but) it’s more complicated when we’re dealing with people and systems.”
So, she transitioned into community health, where she continues to be heavily involved. Now the executive director of Black Creek Community Health Centre (BCCHC), Prescod confronts systemic issues head-on. When northwest Toronto was devastated by COVID-19 during the pandemic’s first wave, BCCHC opened the door for discussion on how marginalized communities are left vulnerable in situations of crisis. However, Prescod says COVID only highlighted the already existing problems at large.
“There are communities with higher rates of chronic diseases such as diabetes that are manageable through proper access to nutritious food, safe jobs, affordable housing and access to care,” she says. “And some people, for some reason, did not and still do not have that equitable access to care.”
Prescod says feelings of anger and disappointment have set in as she watches disadvantaged groups continuously be ignored. She says it’s upsetting and wonders, “Why are they still at the back of the bus?”
“We deserve better,” says Prescod.
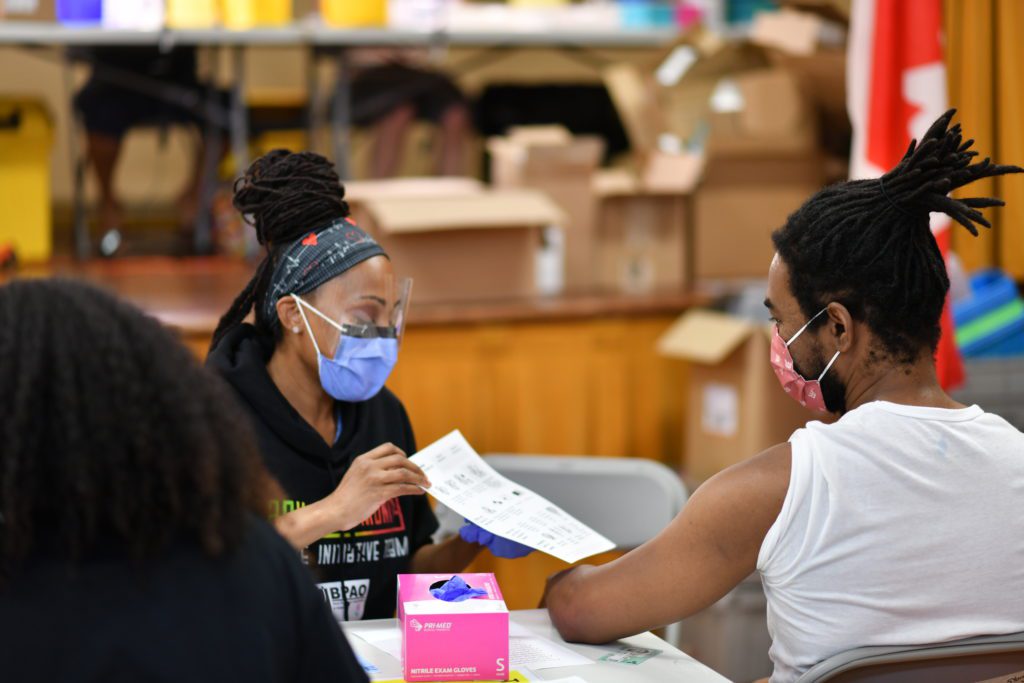
Sitting down with the University Health Network, Prescod and her team advocated for vaccines for hotspot areas in northwest Toronto. While the initiative started off small and consisted of a handful of volunteers at a couple of pop-up clinics, it blossomed into around 50 people and agency partners helping out at multiple locations.
“They were vaccinating thousands of people every day and it was just phenomenal,” says Prescod.
From April to May, Prescod estimates that about 50,000 people received their first dose of a COVID vaccine through BCCHC’s community-based pop-up clinics. While most visitors came willing to get the jab, some needed a bit of a pep talk. Prescod says one Black man in particular shared his fears about the Moderna vaccine.
“He asked if it’s OK. He’d heard it will kill us African people,” says Prescod. “I was able to tell him honestly that I had the Moderna vaccine, and based on what I know, it is just as safe as Pfizer. We interacted and he said he drives a garbage truck (…) and he’s really afraid of getting COVID because he goes to so many places, touches so many things. I was able to convince him to take the vaccine.”
Prescod says most individuals, regardless of race, gender, social or economic backgrounds, are like-minded and are willing to come together in trying times. She and her team want to continue working with communities like those in northwest Toronto and promote viewing decision-making through an “equity lens.”
“Social exclusion can lead to poor health, especially mental health issues.”
“Folks think that some people in certain communities are lazy and on social assistance because they want to be, but no one wants to be poor,” says Prescod. “No one wants to be jobless. There are structural issues that prevent them from getting to where they should be. This is part of a bigger problem within our systems.”
Prescod emphasizes the importance of the health-care system building trust with members of marginalized communities – especially given the prominence of vaccine hesitancy within them.
“Just making that breakthrough with a Black male (…) that’s a success for me, because that’s a population group with a high level of distrust in our system,” says Prescod. “Because he’s going around, he’s heard that this vaccine kills his people, and we have to spend the time to have these conversations.”
At the BCCHC community clinics, Black physicians participated as vaccinators in an attempt to build back trust. Prescod says it’s important for their physicians to be able to talk to individuals in full confidence, know the language they speak, and look like them as well.
“It’s gotten around in the community that some of our physicians are Black – there’s one with dreadlocks – and people come and say, ‘I want that person to vaccinate me.’ It makes a difference,” she adds.
While Prescod has both witnessed and experienced her fair share of discrimination in Canada, she says she will continue to push for policymakers to “understand how to engage with the people they’re serving, and (who) they’re meant to protect.”
“The fact is that, yes, there is anti-Black racism, there’s anti-Indigenous racism – and members of these groups have been the most disproportionately impacted by the pandemic.”
This profile was published as part of the Pillars of the Pandemic series – brought to you by the Dalla Lana School of Public Health and Closing the Gap Healthcare. We will release new profiles in the coming weeks, with 13 people being honoured in total.




The comments section is closed.