Technological advances – including bras that can detect tumours and DNA samples to assess risk – may soon provide inexpensive, non-invasive ways to screen people for breast cancer in their own homes or even while walking to work.
Last year, I received a large envelope in the mail about a breast cancer screening study called PERSPECTIVE Integration & Implementation (I&I). From home, I provided a saliva sample, gave access to my mammograms and answered questions about my family history and lifestyle that were analyzed by a computerized risk-assessment tool. By return mail I was told I was at “high risk” for breast cancer.
When interviewing PERSPECTIVE I&I co-investigator Jennifer Brooks for this article, I disclosed I’m in her study and that’s how I found out I’m high risk.
“You had no inkling before?” she asks.
“No, none at all. I would have bet a million dollars,” I reply.
About one in eight Canadian women will develop breast cancer during their lifetime and one in 33 will die from it, estimates the Canadian Cancer Society. Breast cancers, which men also get, are more likely to be treated successfully when detected early.
Breast cancer risk is based on family history, genetic makeup, personal and medical history and lifestyle factors, says the PERSPECTIVE I&I material I received. Genetic mutations – such as BRCA genes – are rare, occurring in less than one per cent of the population. However, there are variations in genes that are more common to breast cancer – more than 300 of them, explains Brooks. Each gene variation on its own is associated with a very small risk, so the variations are combined into a risk score. This score is added into a risk prediction model that includes other information – family history, mammogram results and lifestyle information – that are all combined to estimate individual risk.
The goal is to refine screening approaches for the general population, says Brooks. Right now, women turn 50 and start having mammograms. If the new risk-assessment tool can identify women at higher or lower risk for breast cancer, it might be possible for them to be screened more or less, based on their risk.
“There’s an international effort … to address the potential for risk-stratified screening compared to a largely age-based approach,” says Brooks. “We can use simulations to model different screening scenarios, where perhaps some women start screening at 40 and others could wait until they turn 60.”
But risk-stratified screening implementation is challenging. In a recent study, Brooks and other researchers found that most women (85.9 per cent) would accept an increase in screening frequency if they were at higher risk, but fewer (49.3 per cent) would agree to a reduction in screening frequency if they were at lower risk.
There is always a balance, Brooks says, between catching and diagnosing breast cancer early so we can treat and improve outcomes versus a false positive that leads to subsequent screening, ultrasound or Magnetic Resonance Imaging (MRI), then a biopsy, only to find out everything is fine. It’s a scary time for people when they think they have breast cancer, she says. A risk-based screening approach is expected to improve the benefit-harm ratio of breast cancer screening programs.
Someone who is high risk, like me, has a greater estimated lifetime risk of developing breast cancer (up to 85 per cent) than the general population (10 to 12 per cent). High-risk candidates are referred for MRI, which addresses some of the screening limitations of mammography for women at high risk, Cancer Care Ontario tells health-care providers on its website.
However, as a screening tool, MRI is too expensive to use widely in the general population, says Elijah Van Houten, a mechanical engineering professor at Université de Sherbrooke in Montreal. But what if a bra, using “elastography” and taking images like an MRI, could detect breast cancer?
Breast cancer tumours are incredibly stiff compared to normal tissue – “Women feel tumours in their breasts,” says Van Houten. In his lab at the university, Van Houten and his team are working on a prototype of an elastography bra, which would take images of the stiffness of the breast. Elastography is an imaging technique that looks for differences between soft and stiff tissue and provides a contrast mechanism to see breast cancer, he says.
Van Houten says the emergence of smart textiles led him to think: “If garments are getting smart, then why don’t we build something that’s able to take the data that I need, to take these images that I need, because then the woman just wears the technology. She’d be taking images all day long!” His excitement is palpable.
The more images the better, he says. The bra, which generates high-quality images, would provide a rich data set, in a convenient and inexpensive way, to extrapolate the information needed to see the stiffness of the breast, and therefore the presence of cancer tumours.
“What we’re trying to do is bring the (imaging) technology that is currently only really available on the MRI to be much more accessible to women,” he says.
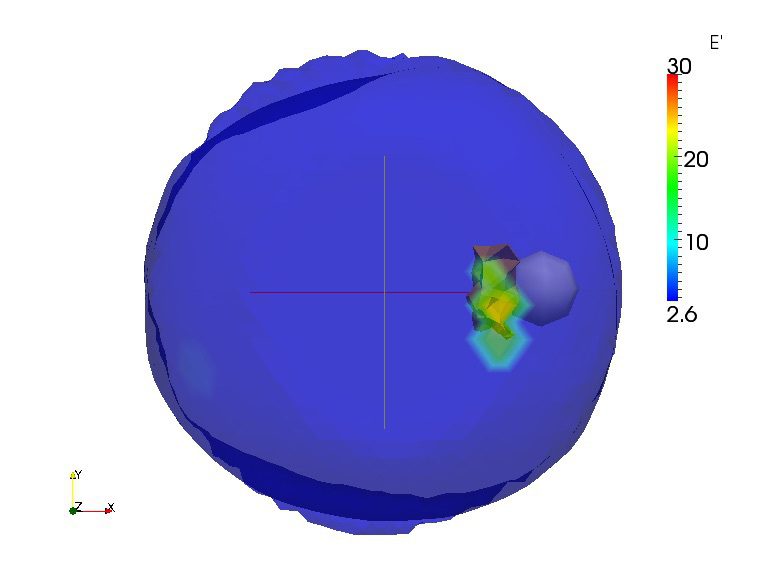
A picture of a breast containing a lump of stiff tissue visually represented by the elastography-using bra.
Elijah says the bra prototype will be tested next month. In the coming years, it could be used to screen women with dense breasts, at high risk for cancer or already in breast-cancer treatment to see if chemotherapy or radiation is working to reduce the size of tumours.
In another part of the country, a physicist is also trying to develop a way of finding early signs of breast cancer. Having dense breasts is a known risk factor for breast cancer, which means you have more milk glands, milk ducts and supportive tissue than fatty tissue in your breasts. Mammography, which looks at breast density, is currently considered the most reliable method of finding breast cancer.
But breast density can be normal or cancerous, says Alla Reznik, a Canada Research Chair in Physics of Molecular Imaging and a professor of physics at Lakehead University in Thunder Bay, Ont. Because dense breast tissue can hide cancer, mammography is no longer considered the gold standard for women who have dense breasts or who have been identified as high risk, she says.
Reznik and her research team at Lakehead are using positron emission mammography (PEM) to improve accuracy of breast-cancer detection at earlier stages for women with dense breasts.
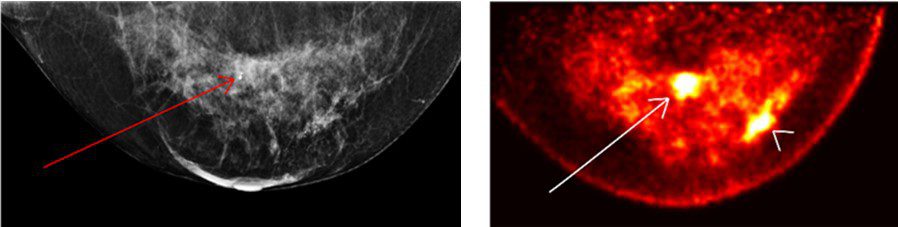
These are images of the same breast, with an X-ray mammography on the left and PEM imaging on the right, from a 56-year-old patient with invasive ductal cancers and two histopathology-proven lesions.
With PEM, it is much easier to find these lesions, says Reznik. Even with a retrospective look at the mammography, she says, you are unable to identify the second lesion in the dense breast tissue, but with PEM it’s very clear (see image).
PEM is also less painful for women because it does not need the strong compression used in mammography, says Reznik. PEM is a molecular imaging technology that detects radioactive glucose, injected intravenously. “Cancer cells love glucose,” she says.
When radioactive glucose is injected, the cancer cells become more radioactive than surrounding benign tissue, allowing them to be captured by the PEM detectors. More glucose uptake is a direct identification of most malignancies, Reznik says. The PEM scanner uses the same dose of radioactivity as mammography.
“For patients for whom mammography is inefficient due to radiologically dense breasts, we perform much better since high sensitivity of PEM does not depend on breast density. In addition, our specificity for breast cancer is much higher than MRI,” says Reznik.
Contrast MRI images can be misleading, she adds, producing false positives that can lead to unnecessary biopsies or mastectomies, whereas PEM directly shows cancer cells that have absorbed radioactive glucose.
Reznik is seeking funding to conduct clinical trials on her technology. If you have breast cancer history in your family, and you have to make a decision about removal of breasts, she says, let’s use a test that is very simple, not invasive, and not painful.
What if a bra, taking images like an MRI, could detect breast cancer?
If people are at high risk due to family or personal history, would they also be interested in additional genetic information about other diseases they may have, or are predisposed to get?
If you are at high risk for breast cancer you may qualify for genetic tests. (After speaking with a genetics counsellor and providing additional family information, another risk calculation was done, and I did not qualify for the testing.) Genetic tests typically look at a selection of genes, mutations and variants that are associated with targetable cancers, says Yvonne Bombard, a genomics health services researcher and scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto. However, when you move into her field of sequencing technology, she says, a genomic sequence panel can reveal information about your entire genetic makeup, called incidental findings.
Bombard’s new GENOMICS ADvISER app will help women who are offered these incidental findings make an informed choice about which of them they might want to learn about. Incidental findings are additional genetic information, unrelated to your current condition. For example, through the app women in Bombard’s studies (largely from the breast cancer community) could choose to learn about their risk for other diseases such as diabetes or Alzheimer’s. Or some women may find it too stressful to know.
In an initial trial, patients found the app provided better education and a higher level of satisfaction than talking to a genetic counsellor, says Bombard. Currently, a trial is underway to find out what patients want to learn about their incidental genetic findings, the benefits and risks of finding out more about their potential risks – does it cause distress? does it change behaviours around screening, surgeries, diet and exercise? – and the cost to the health-care system of sharing this information with patients.
“Wouldn’t it be nice, at your own leisure, to open up a well-designed digital platform and, at your own pace, learn through videos and synthesized content, and have this supportive, engaging platform to deliver all this rather complex information?” asks Bombard.
To this and other technological advances, I say: “Yes.”


The comments section is closed.