Hello, dear reader!
This is my first column for Healthy Debate as a Patient Navigator. This column will be devoted to providing patients with information to help them through their journey with the health-care system and answering your questions.
Here’s a bit about me: I have been a patient partner at The Ottawa Hospital and Ottawa Hospital Research Institute since 2017, and have joined a variety of governance boards that work on patient and caregiver engagement such as the Patient Advisors Network, the Ontario Health East Region Patient and Family Advisory Council and the Equity in Health Systems Lab.
My journey as a patient partner started much before 2017 though. When I was a teenager, I was diagnosed with a cholesteatoma, a rare and chronic disease that causes the development of fatty tumors in the middle ear. I have had multiple surgeries to try to fix it but will need regular follow-ups to monitor whether the tumor returns. Because of this, I also live with an invisible disability since I have essentially become functionally deaf in one ear and often rely on a hearing aid when I navigate the world.
Having undergone three surgeries in my adolescent years, it was my experience undergoing surgery for an acute hand and wrist injury following a jet ski accident as an adult that was the catalyst for my decision to become a patient partner. There was an intriguing contrast between how I was cared for at two different health-care institutions, my age being the deciding factor at which hospital I went to (a children’s hospital or an adult one).
The most memorable example was how, as a teenager or child, you were never left alone before surgery, and nurses and staff took all the time necessary to comfort me and answer my (and my family’s) questions. I also remember how right before putting me to sleep, the whole staff initiated a surgical pause and introduced themselves and explained to me what their role was during my surgery.
None of that happened as an adult. I was left in a hallway while the operating theater was prepared, anxious and alone with staff walking by not even batting an eye. My questions felt like an annoyance to the care team; as soon as I was wheeled onto the operating room table, the anesthetist quickly put me to sleep. I didn’t even have the time to see who else was there.
Now don’t get me wrong: I am incredibly appreciative with the quality of care I received, but it was the everyday interactions with the care teams that I felt could be improved. And so, while I was recovering from that surgery, I looked for a way to help other patients and the hospital improve its care. I discovered the hospital’s patient engagement program, applied, and the rest is history!
Since then, I have worked on a host of patient-centered policy and research projects and fervently advocate that surgical teams adopt a more compassionate approach with patients before and after surgery.
I’d be happy to talk a bit more about my journey if you ask, but with that out of the way … Welcome to our first patient navigator column about patient engagement.
Conceptualizing the continuum of Patient Engagement
In the context of Canadian health care, patient engagement is a multifaceted concept that involves active collaboration between patients, caregivers, health-care providers and researchers. It involves patients and caregivers as active contributors in decision-making processes, health-care services and medical research. Though the concept is not new, the paradigm shift toward patient engagement in Canada started around 2010.
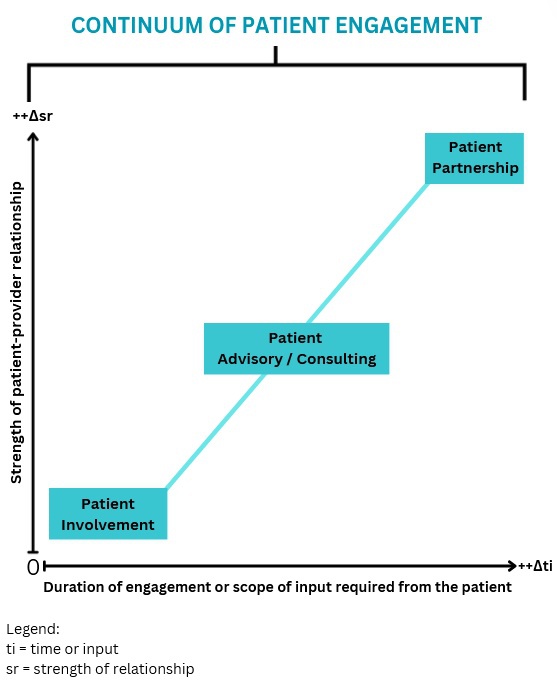
I like to conceptualize the different levels of patient engagement as a measure of the strength of the relationship between patients and their interlocutors – whether it’s a healthcare provider, administrator or researcher – charted against the duration of the engagement or the scope of input required from the patient (Fig. 1).
Figure 1: Continuum of patient engagement (Lê, 2024).
Defining different levels of Patient Engagement
Following the continuum, let’s begin by defining different levels of patient engagement. Bear in mind that these definitions can vary from one organization to another but are useful in generally labelling the level of patient engagement a project has achieved (or wishes to achieve).
Patient involvement: If the strength of the relationship between patients and their interlocutors is minimal and not time consuming or too onerous, then perhaps it can be categorized as patient involvement. This applies to many instances of transactional engagement.
Patient advisory/consulting: Right in the middle of our continuum, patients can find themselves engaging in patient advisory or consulting work, where projects are limited in scope and duration or complexity, and the relationship is not as profound as a partnership.
Patient partnership: The stronger the relationship is between the patient and their interlocutor, and the longer the engagement activity lasts or how much input the patient is providing, the more this situation can be categorized as patient partnership. It is the inverse of patient involvement.
Examples of the different levels of Patient Engagement
Let’s pretend you are accompanying a loved one to an appointment to manage a kidney disease, requiring them to undergo dialysis treatment. We’ll use this scenario to exemplify what label could be used to describe the level of engagement.
Patient involvement: In our case, if your loved one – or you – fills out a satisfaction or feedback survey about your experience in the waiting room and all that needed to be done was to hand it back to the clerk or care team, then, at a basic level, you could likely label this interaction as a form of patient involvement. It can also involve open consultations around a design of a new look and feel for a hospital, or the understandability of a survey or communications product. Interactions with the care team, administrators or researchers are minimal and often transactional.
Patient advisory/consulting: If your loved one was asked for more detailed information about survey results over the course of a few meetings, this could represent patient advisory/consulting. This could mean that patients meet with program administrators and care providers and share their insights on how things can be improved. It essentially involves patients providing advice to health-care institutions from the perspective of patients, their family members and caregivers.
Patient advisors or consultants are often appointed by hospitals or academic institutions to offer insights at multiple stages of health-care delivery and research. They can help pilot an initiative based on that feedback or evaluate whether the new solutions are working. Often patient advisors are engaged in smaller-term individual projects and meet with the project team as regularly as required.
Patient partnership: Going above and beyond patient advisory, if patients have built a trusting relationship with their care team or administrators, they could feel comfortable enough to partner with them and initiate a project of their own. This could be for a project in which they study a different form of treatment to improve patient-centered outcomes (like the time it takes to feel “normal” following a session); it could be working together to identify and remove barriers for other patients that need to access that type of care. These projects are not fulfilled overnight, but require a collaborative, longstanding and trusting relationship between patients and health-care providers, administrators or researchers. It ensures that patients, regardless of severity or chronicity of their illness, can meaningfully contribute their experiences to aid in improving patient care, or develop or implement policies, pilots or research projects from start to finish.
It is leveraging that lived and living experience to its full extent and having the patient partner involved as an equal voice in the decision-making process for a project – over many months, usually – that the engagement could be labeled a partnership.
Last words
The point of this column will be to answer or explore issues or questions related to patient engagement, health communications or even provide some thoughts on how to handle a particular situation.
I would be happy to collect your questions and feedback at any time, which will help inform future columns. Just email me at max@le-co.ca or connect with me on social media (Linked In, X / Twitter).
It’s not easy to navigate our health-care systems, but you are not alone.


The comments section is closed.