The sudden decline in diabetes screening as a result of the pandemic has put a significant number of Ontarians in danger of vision loss.
The COVID-19 pandemic revealed multiple strained layers of the Canadian health-care system and its delivery, with care coordination and access among the top concerns. Two-thirds of Canadians living with a chronic illness have faced challenges accessing treatment and care. According to a report by HealthPartners, 30 per cent experienced a cancellation of screening and diagnostic appointments and 43 per cent had a cancellation or delay in their treatment. Chronic disease screenings took a back seat, including diabetic retinopathy (DR) assessments that plummeted during the early phase of the pandemic. These delays have had a negative impact on patients’ quality of life.
1 in 9 Canadian adults are diagnosed with Diabetes Mellitus
549 new cases diagnosed daily
20% – 65% Canadians not screened for DR
The Canadian Institute of Health Information (CIHI), Canada’s government-funded health data and statistics agency, recently reported that diabetes mellitus (DM) is one of the three most common chronic diseases in Canada. It is a growing burden and continues to put pressure on our health-care system with an average increase of 3.3 per cent in the number of people diagnosed with diabetes every year.
Diabetic retinopathy (DR) is one of the most common complications of this chronic disease. People with DR form the bulk of candidates for vision loss and is the leading cause of blindness in people of working age. A recent study in Ontario revealed the sudden decline in diabetes screening due to the pandemic, anywhere from 20-65 per cent based on age groups and income. In 90 per cent of cases, catching the unscreened early and performing regular eye checkups can prevent severe retinopathy conditions. Unchecked, this problem is associated with a massive cost for the government and society. Treating a patient with retinopathy can cost anywhere from $3,000 to $11,000. This can be avoided with a proactive screening strategy.
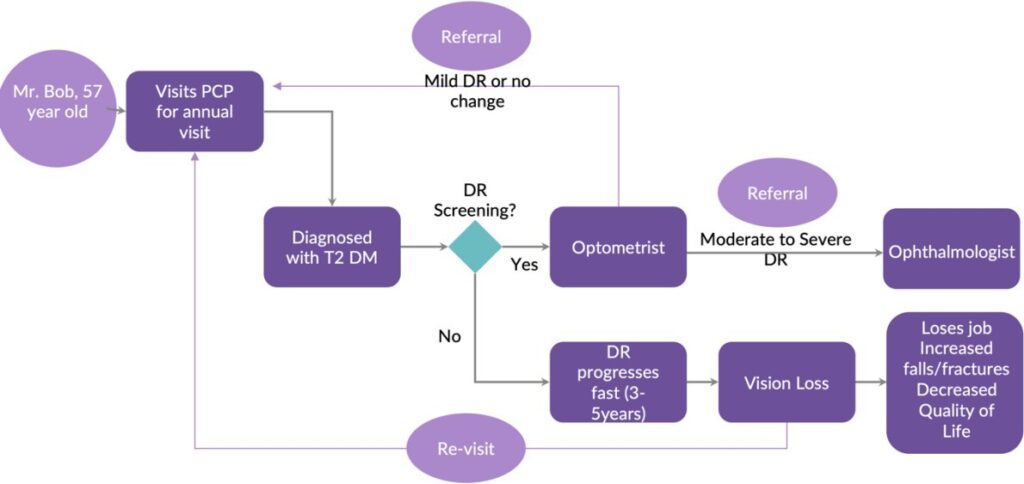
Let’s take a look at a patient’s journey:
Bob, a patient with diabetes, is advised by his doctor to complete a retinopathy screening at the time of diagnosis. However, this is generally verbal advice. There is no formal, structured system for referral and follow up with an optometrist. A bidirectional flow of health information is vital for a family physician to offer continuity of care to patients. Lack of information exchange between clinicians has resulted in no less than 400,000 unscreened patients with diabetes in Ontario. Evidence suggests that strategies that increase uptake of screening appointments can reduce the risk of onset retinopathy. Clear communication and real-time inter-professional collaboration in primary-care settings can prove eye-saving, and this can be driven using digital health solutions.
“In the early stages of diabetic retinopathy, there may be no symptoms which is why it is especially important for people living with diabetes to have regular eye exams,” says Jan Hux, President of Diabetes Canada. – International Federation on Ageing
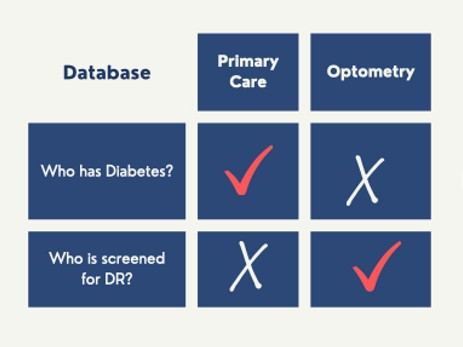
A disconnect in information sharing is costing Ontarians
Data about screened individuals is siloed and trapped in patient records. If a patient consults an optometrist for retinopathy screening, the screening status is recorded in the optometrist’s electronic medical record (EMR). Documentation of this information rarely makes it back to the family doctor. Data may be shared within an integrated practice that comprises physicians, optometrists, and ophthalmologists, but this is a rare combination in Ontario. Populations with lower social determinants of health, gendered individuals, Indigenous populations, young adults, immigrants, those not under the care of family physicians, as well as racialized and ethnic marginalized populations such as Black, Asian, Middle Eastern and Hispanic people are the most likely to miss being screened.
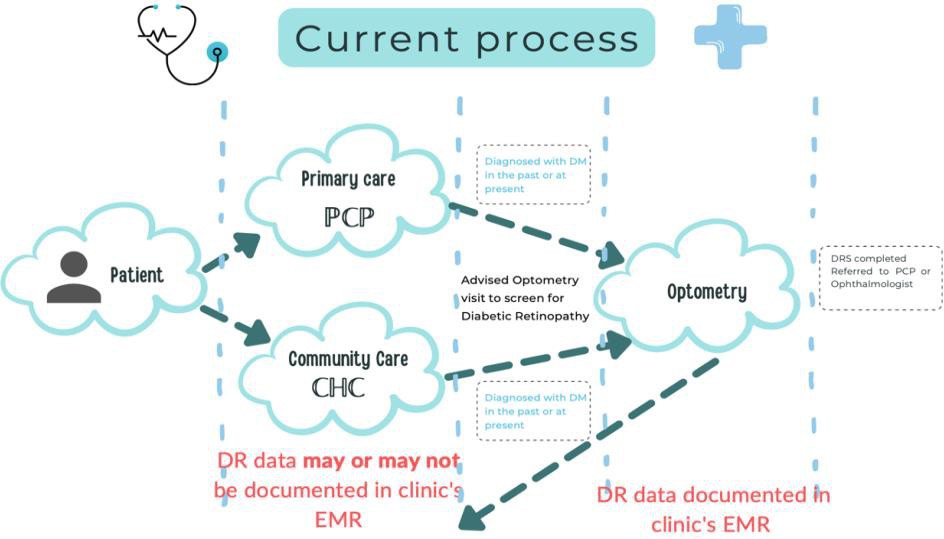
Optometrists play a crucial role in a diabetic’s circle of care. Exchanging the relevant data from an optometrist’s EMR to a family doctor’s EMR can save thousands from severe retinopathy.
Interoperability and data exchange is possible using clinical communication and collaboration tools that are now increasingly used in practices. Communicating a patient’s screening status to the family doctor will enable tracking of unscreened patients who can then be informed of the need to visit an optometrist. Tools such as eReferral, Secure-Mail and Health Report Manager, which already exist in Ontario, can enable optometrists to share a patient’s screening data.
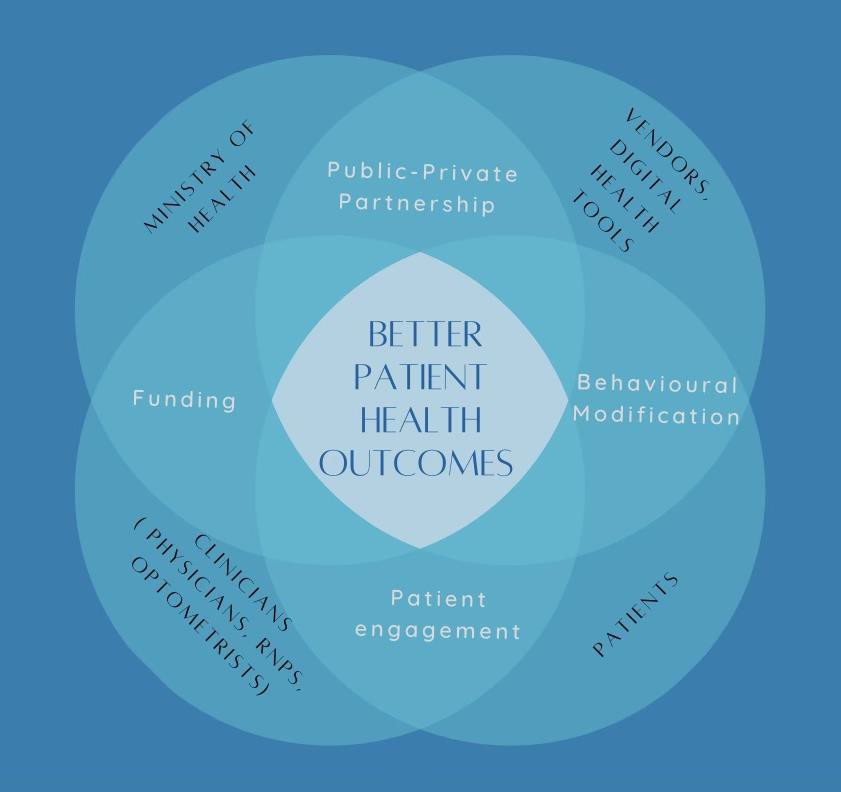
Recently, the Ontario Health Data Council shared a report with recommendations for responsible use of health data to establish a sustainable, learning health-data ecosystem that benefits the people of Ontario. Our use case fits its vision and system-level recommendations such as an integrated and accountable care approach between providers of different care settings; population health management that identifies specific strata of our society; and the unique needs of patients with diabetic retinopathy. An interoperable digital tool that connects physicians to optometrists and vice-versa will enable timely retinopathy monitoring and management.
Nevertheless, challenges persist in implementing interoperability due to reasons beyond technology, such as health system policies, incentives, user adoption and influence of governance and regulatory frameworks.
We recommend that Ontario Health prioritize this simple form of interoperability between optometrists and family doctors. The cost will be low, since only three or four pieces of information need to be shared. Adoption will be relatively easy for both parties for the same reason. The benefits will be in the hundreds of millions of dollars, since the number of patients affected is very high.
Saving money by providing patients with high quality care is possible. High rates of screening for diabetic retinopathy have been achieved in England and Scotland to great effect. It’s time Ontario became one of the success stories.


The comments section is closed.
Certainly needed but in our current system this will create more work for providers—reviewing reports, documenting, searching overall practice stats, contacting pts, and making referrals. We need universally accessible data (including by pts) and automated workflows/ notifications.