Ontario’s Health Links initiative is a “big manoeuvre” in a complex provincial system, acknowledges Helen Angus, associate deputy minister with the transformation secretariat of the Ministry of Health and Long Term Care (MOHLTC).
The initiative aims to facilitate coordination of care at a local level for high needs patients. It comes in the wake of the province’s primary care reforms and the introduction of accountability agreements with hospitals.
After a selection process in late 2012, the ministry received business plans earlier this month from the first 19 of an anticipated total 77 Health Links.
Hoping to provide better care for the top 1 to 5% of users
One of the goals of the initiative is to provide better care for the 1% to 5% of citizens who, research has indicated, are high users of health care. The focus is to be on the subset who are high users with multiple chronic conditions and on senior citizens. The definition and identification of high users will vary at the local level but might include, for example, a person with severe heart failure and chronic obstructive pulmonary disease who has early dementia.
It also aims to reduce costs, particularly expensive hospital visits, based on the assumption that many of these patients’ hospital emergency ward visits, admissions and re-admissions, can be prevented with better coordinated care.
Approximately 50,000 citizens are expected to be covered by each Health Link—though the population totals vary—and each Health Link reports to its Local Health Integration Network (LHIN).
The size and number of the Health Links is based on research by the Institute for Clinical Evaluative Sciences (ICES) that identified natural referral patterns between doctors and hospitals in local areas. The Health Link is supposed to provide a governance model, and a political push, for the ICES-identified groups to work together.
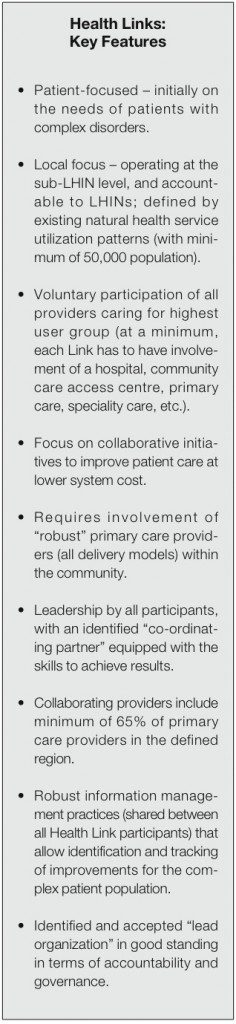
All Health Links are required to have physician involvement. The OMA has indicated support for the model and recently provided its members with a summary that is reproduced in the attached box.
This information first appeared in the February 2013 issue of the Ontario Medical Review and is reproduced with the permission of the Ontario Medical Association.
A focus on coordination
Need for more coordination is evident, as the fragmentation and disconnects in the province’s health care system are obvious to many users. “Many patients are left to navigate the system alone, seeing a myriad of unconnected providers, who are unaware of patients’ past experiences, leading to duplication of diagnostics and care,” the ministry notes in a background document on the Health Links initiative.
The push towards better local coordination of care for high needs “complex” patients is being launched concurrently with health system funding reform and austerity measures.
Still, most observers applaud the intent of the networks, though they emphasize that “the devil is in the details”, and some warn that the limited development funding for the local groups—capped at $75,000 each—may prove inadequate to the challenge. (Once a plan is in place, each Health Link may receive up to the $1-million in one-time funding.)
The Health Links initiative, which is based on voluntary participation, is modelled in part on accountable care organizations in the United States, and similar groupings in the United Kingdom and Australia and New Zealand.
While each Health Link has to provide baseline data and develop measures that will allow for evaluation of the initiatives, the emphasis is on better information sharing and on innovations that allow providers to respond to local needs.
Privacy concerns about health professionals sharing patient information should not present a barrier as these issues have been clarified by the information and privacy commissioner of Ontario, Angus notes.
Further, a team within the health ministry is committed to responding in a timely fashion when individual Health Links identify real or perceived barriers to better coordination of care, she says. Barriers might include, for example, policies that appear to unreasonably limit home care for post-acute care or palliative patients. The ministry’s response will indicate how the barrier might be removed and while eliminating some barriers could be relatively straightforward, removing others could involve regulatory or legislative change, Angus noted.
Guelph and Temiskaming among the early adopters
One of the 19 “early adopters” is a Health Link led by the Guelph Family Health Team (FHT) which, with 75 doctors as well as nurses and other health professionals, provides health care to about 100,000 of the city’s 120,000 citizens. The group’s steering committee includes the police chief, and representatives from the local hospital, the children’s aid society and the local community health centre.
Patients who incur high costs and could benefit from more coordinated care are being identified by reviewing their primary care medical charts, says Ross KirkConnell, executive director of the FHT.
He cites the example of a patient with several mental health issues and a limited income who can’t afford to get to the family doctor when symptoms become overwhelming, and so opts to take an ambulance to the hospital emergency ward.
A different way of providing care for such a patient could better suit the person and also reduce ambulance and hospital costs, he notes. “The challenge—and this is a system challenge— is not to be health care centred but to also look at poverty, transportation and disability issues,” he adds.
In the beginning, Angus does not anticipate that funding will be re-assigned among providers and agencies, but rather that they will be more aligned, and work together. “If a big improvement is demonstrated,” she said, there may in the future be an opportunity to redistribute money upstream to, for example, better housing for a high needs patient.
The Guelph Health Link aims to assign one person in primary care, likely a doctor or a nurse, to be the “go-to person” who can keep in touch and intervene as necessary on behalf of each patient who is deemed high needs and would benefit from more coordinated care. “’If there was just someone I could call’ is a statement that we hear from patients a lot,” says KirkConnell.
The approximately 33,000 people in the Temiskaming Health Link, another one of the 19 who submitted a business plan, are spread out geographically and represent diverse populations (about 24% of the population is French speaking and 8% are First Nations.)
The Health Link is led by Le Centre de santé communautaire du Témiskaming and membership includes three hospitals, four other community health centres as well as the Northeast regional Community Care Access Centre, the public health unit and representatives from the Canadian Mental Health Association and seven local nursing homes, says Jocelyne Maxwell, executive director of the CHC.
Maxwell explains that a group called the Temiskaming Collaborative Health Providers predated the call for the formation of health links. The group’s aim was to better coordinate care and, although all were health providers, “we spent a good year just trying to understand what each other did,” she said.
The group had launched plans for joint human resource plans, and welcomed the Health Link initiative, because it provided an initial target patient population to focus on. “The exciting thing about Health Links is that it forces us to step back and really think about how to provide health care differently, as partners in a system with joint responsibility.”
Importantly, patients are included in this process, she says. “After all, they are the ones who can best identify the challenges they face.”
Scaling up across the province will be a challenge
Rick Glazier, who co-authored the ICES research (not yet published) that laid the groundwork for the configuration of the Health Links, said the main challenge facing the voluntary organizations will be to prevent unnecessary, costly hospital admissions. “Let’s face it, preventing one visit to a primary care practitioner is not going to save much money.”
Getting providers together to improve the quality of care is a great ideas, says Adalsteinn Brown, Director of the University of Toronto’s Institute for Health Policy, Management and Evaluation. The challenge will be “what to do next, how to get from one side of the province to the other—how to scale up— and how to get the evidence base” to support an authoritative evaluation.


The comments section is closed.
I am the Director of a small rehab agency in Durham region which has P;hsyiotherapy, Occuapational Therapy, Social Work and Dietitians (contracted to the CECCAC). Also I am the Director of an Out patient clinic in Pickering that has physiotherapy, kinesiology and massage therapy. In total, we have about 38 therapists. Would Healthlinks be an organization that I should be interested in joining or submitting a business plan or are my two agencies not expansive enough. I was recently at the OHCA symposium and I heard the Deputy Miniser speak about Healthlinks and it was a very interesting approach to linking up organizations.
Hi Angela,
I’m not sure exactly how the Health Link in your area is shaping up. I suspect your organizations would be too small to be a lead for a new Health Link, but the existing Health Link in your area may be keen to have you join, or they may know if another Health Link will be starting closer to your location in the near future. I believe the first Health Link in the Central East LHIN is in Peterborough, but there are plans to roll-out several more. You may wish to contact your LHIN or the Peterborough Health Link: http://www.centraleastlhin.on.ca/report_display.aspx?id=24968
Best,
Jeremy
I agree with Sharon Wilton’s comments that the concept needs to be broadened and that we cannot rely on a “top down” approach. Sharon’s point of broadening the scope by creating an ‘alliance of advisors” and “encompassing the wider arena of population health” is absolutely right on.
As an Occupational Therapist who has dedicated my professional career to people with complex neurological conditions and keeping them out of hospital, I am thrilled to see this conversation finally taking place. My colleagues and I have built a unique and innovative interprofessional community service for people with very high needs and complex neurodegenerative diseases that addresses the medical, non-medical and social determinants of health. We have incorporated exactly the kind of integrated “client to program” model that Sharon suggests and are also adept at using the OTN model that Dr. Meloff is suggesting to reach vulnerable and marginalized clients. I am hopeful that those of us in the neuro-rehabilitation field will be included in this conversation so that we can share our findings and help build capacity and a sustainable system of care for those with complex needs.
Respectfully submitted,
Pearl Gryfe
pearl…
“Inter”professional teams form an “alliance” with each other( preferably P3) that includes the client “person” as recipient and reporter. Technology facilitates this.
The PDAG ( Program Design “Advisory” Group) is multidisciplinary and functions as apomediator ( nearby on standby for “department” assistance ) also includes the client “person” as advisor .
Restructuring the LHIN facilitates this.
The one stage in alliance formation the LHIN has to face is ” divestment” in order to become a viable program with stand alone survival skills in terms of design.
[ it would be great if we had a file section here to send details :) ]
As the new Professional Leader for Social Work at Sunnybrook Health Sciences Centre, I am thankful to participate in some Health Link strategies to meet “complex patient” care needs and collaborate with system partners. One aspect that would benefit further dialogue would be to develop a better integrated conceptual framework of “complexity” that not only includes medical markers or # of visits to the ED but biopsychosocial indicators that are often out of the control of patients and their families but crucial points of further analysis and leverage points in developing responsive person centered care delivery. Look forward to the ongoing commitment and collaboration.
Respectfully, Lina Gagliardi
In reading the ” preliminary step ” accepted Business proposal that includes Temiskaming I am looking for:
The Business Case
Preliminary proposal step:
A Strategic Investment approach (with interdependent skilled professionals ) aimed at “ building capacity” in:
• Accountability measures
• Governance
• Community Service development
• Program Management capability
• Technical capacity
What I don’t see in the application is any reference to to the much touted ” strategic investment” of approach of ” building capacity ” which is more than rearranging the parts that impact the medical determinants of health .
i.e. The thrust of medical, nonmedical ,AND social determinants of health in the “transformation” perspective is not expressed in the membership group.
excerpt:
‘ The plan focuses primarily on transitions of care, breaking down funding barriers, eliminating duplication and the creating formal care pathways across the continuum of care. Inherent in the plan is the need to involve, patients, clients, families and caregivers in the model development. ‘.
Membership:
Temiskaming Hospital
Kirkland Lake Hospital
Englehart Hospital
Temagami Family Health Team
Great Northern Family Health Team
Haileybury Family Health Team
CMHA Timmins and Temiskaming Branch
Timiskaming Health Unit
Temiskaming Home Support
Temiskaming Palliative care
Centre de santé communautaire du Temiskaming
North East Community Care Access Centre
Temiskaming Lodge
North East LHIN
end of excerpt
Considering a SWOT of past performance and practice models inside the multiple ” good ideas” that emerge from a top-down perspective ( e.g. will we ever forget ” one-stop access” ) personal interviews with participants revealed a failure of the ?concept to proceed after pilot.
That failure was best described as “no secondary event structured to proceed with local implementation”(hospital CEO comment).
However grand these concepts are in their ” all encompassing” description of better client connection and subsequent service delivery models they fail in performance when the focus is a” top down” start [ versus multiple focal points that animate governance, workers, and clients ( now clustered under the title ” person”) ].
One suspects the true purpose of the concept is actually to cluster an “inter”professional team to design effective Carepaths for predictable disease states ( in preparation for the ICD-10 expansion into 45,000 more codes by 2015 ).
There is nothing wrong with that goal but it is too narrow in it’s perspective and could endanger client /worker participation if their own goals are not incorporated into “first steps” action.
The buffer zone in the “community-as-partner concept ” is not best served by design emerging from”established programs” or ” emergency programs” the stress adaptation needs are broader)
To use Health Links initially as a portal of activity ( from which a Primary Care model emerges ) should be considered with:
(a) open entry once the gate is defined;
(b) distribution of entrants into “skills training ” or ” service application”;
(c) incorporation of programs designed that links “CAREpath” to CASEpath.
This implies and undergirds a notion that the Carepath /Casepath construct is of little value without a defined Workpath and can only be overcome if there is companion activity in the design of all 3 ( from onset ).
There is no longer any turf to war over. Clearly defined parameters of payment demands clearly defined avenues of “to” whom and “by” whom. Who would want the skillbase of the professional knowledge worker to be replaced by a software equivalent if it is viewed as a “one-off shot “??
Matrix grouping around programs is no longer traversing a horizontal line. It is ” floating in a medium” of P3 options that will:
1. coalesce and cluster around the dominance of “social” clusters… no longer fully dependent upon medical determinants.
2. incorporate the knowledge worker in an oblique connector line joining “client to program” across the multiple program offerings( also “inter”dependent and P3)
I say broaden the scope of the concept of Health Links from this point forward by creating an alliance that looks past established practice of “board” and”head and shoulders” governance…. forward into”advisors” encompassing the wider arena of ” population health” encouraging a free flow reporting of all parts in medical, non-medical and social determinants of health.
I have an elderly friend who had a very traumatic experience with the healthcare system in the late 90’s. What happened to him should not have happened, and I believe that a system such as this could have prevented the harm which happened to him. I think a “facebook like” system for communicating between care providers would be incredible. If the patient, and/or designated caregiver could be able to see the information, and ADD to that information, It would be absolutely wonderful.
I concur with John Moore- it is very difficult to communicate among different care givers
for patients with complex chronic problems. From my personal experience dealing with
“ambuatory” geriatric patients (an oxymoron of ever there was)- that is, frail elderly outpatients seen in
an “ambulatory care centre” all of whom have neurological problems of one sort or another-the need
for interdisiplinary care screams out and is virtually unattainable.
I think Telemedicine would provide an opportunity to overcome some of these issues-the infrastructure exists ( OTN)- the organization and execution of viable effective interdisiplinary “case-conferencing” to render optimal care for the patients, via telemedicine, is missing and is critically needed.
Respectfully submitted, Keith Meloff MD, FRCPC General Neurology Baycrest Centre.
Leveraging the OTN infrastructure for ‘case conferencing’, as Dr. Meloff suggests, sounds like a great idea. This is still, however, ‘episodic’, and I am wondering if there is a way for some kind of ongoing monitoring and sharing- which might alleviate the need for more frequent conferencing, or might trigger the need for a conference at a critical point. Some people have suggested a “Facebook-like” (and not Facebook) application that is monitored by the patient and by the patient’s primary care lead in the Health Link organization, and that is undated by the patient’s multiple providers when they have news. Note that ‘news’ is more than health data (the EHR, eventually)- it is also comments, plans. questions to the group of providers, etc. The idea is to involve the provider team before the patient has a problem and is sent to one of the providers, who then “looks up the record” to see what has happened…
Health Links is an exciting initiative, and a prerequisite for providing coordinated care for high needs patient; it provides the “governance model, and a political push”, as well as the point of connection for the patient to “a myriad of unconnected providers.”
What Health Links, as an organizational/governance model, does not do (yet) is provide the means to connect providers around the care for a high needs patient. I don’t see this as only sharing data (i.e., an EHR) and eliminating duplication- it is about how providers collaborate about the condition and care plan for the high need patient, reacting in real time when something changes or intervention is required.
One way to do this is daily conference calls about each patient- but obviously that will not work. We need to put some effort into defining the process of collaboration, and then determine how to support that collaboration- inevitably with technology.
Health Links are generating an excitment and optimism in the system that I have not seen for a while. I think that is because the goals resonate so well with people in the field who know that care can be better coordinated, and with a focused effort on high needs populations, we will be able to make a difference. Landing the plane in terms of delivering on the potential HL offer is the big test and to help that, we not only need active engagement of clinicians and patients, need leaders coming to the table who are well equiped with experience and skills in change mangment. Being able to mobilizing hearts and minds of diverse stakeholders, is as important as being able to put the evidence to work. Great summary article, thanks.