When Travis Saunders went for his regular physical a few years ago, a nurse calculated his Body Mass Index (BMI). At 24.5, it was at the high end of normal, and she told him to “watch his weight.”
“I just kind of smiled and nodded,” he says. As an obesity researcher, Saunders knew that since he was a competitive runner who ate well, had a stable weight, and was generally healthy, he didn’t have to worry.
He was concerned, however, about the nurses’ advice. She shouldn’t have been issuing such warnings based solely on BMI without discussing any of those other factors. Plus, “telling someone to watch their weight is totally unactionable health advice,” says Travis, who is now an assistant professor at the University of PEI. Wouldn’t it have been better for her to offer him lifestyle advice?
It’s a big question. BMI doesn’t, by itself, mean that you’re unhealthy or sick, and it’s unreliable in many ways – including that it’s not a particularly good indicator of how much body fat you have. So should you be concerned if you fall into the BMI categories of overweight or obese? And should doctors be tracking patients’ BMIs and talking to them about it?
Family doctors’ guidelines for BMI
BMI is used in almost all studies on obesity, partially because it’s easy information to collect and calculate. It has also been used for a long time, so it’s easy to compare new information against historical info – revealing trends like the fact that the number of obese Canadian adults has almost doubled between 1978 and 2011, rising from 14% to 26%.
Those growing rates are a major cause for concern. People who are obese are seven times more likely to develop diabetes than those who have a normal BMI. It increases the risk of heart disease, stroke and heart attacks. And it’s been connected to some cancers, including breast and colon cancers. Almost one in 10 premature deaths of those 20 to 64 years old can be traced back to excess weight.
The connection to health problems is stronger with obesity than it is with merely being overweight, however. And other factors, like how well you eat and how much you exercise, can be equally if not more important than how much you weigh.
The BMI calculation – how many kilograms a person weighs divided by how tall they are in metres, squared – was created by a mathematician way back in 1832. People who have a BMI under 18.5 are classified as underweight; normal BMI is designated as 18.5 to 24.9; overweight is 25 to 29.9, and obese is over 30. Obesity is further subdivided into three categories, class I, II and III. (If you’re curious to know your own number, you can find a BMI calculator here.)
BMI is well-known to be better suited to population-based epidemiology studies than to being used as a screening tool for individuals. Yet according to guidelines released this year from The Canadian Task Force on Preventive Health Care, family doctors should calculate BMI in their adult patients.
The advice to routinely monitor BMI is classified as a “strong recommendation” but is based on “very low quality evidence.” It’s one of the few recommendations that fall into both categories, says Paula Brauer, chair of the Task Force’s adult obesity working group. That’s because there is no research on using BMI as a screening tool, but the group felt that obesity needed to be addressed in primary care. “It’s just logical,” she says. “If height and weight are never being measured at all, then you have no basis for being able to guide a patient.”
The advice goes beyond just tracking BMI, strongly encouraging doctors to refer or offer obese patients who are at high risk of diabetes to structured behavioural interventions. And they offer a “weak recommendation” to do the same to adults who are overweight or obese. Brauer adds that it may be useful for doctors to talk to patients about weight if they’re inching towards the overweight or obese range, since it’s easier to not gain weight than it is to lose it.
The recommendation has caused some controversy, however. One of those who’s come out against it is Yoni Freedhoff, assistant professor of family medicine at the University of Ottawa. “BMI as a tool for family physicians is very poor,” he says. “It’s a measure of bigness – measuring the gravitational pull of the earth. Using that as a surrogate marker of health probably isn’t a good idea.”
‘An imperfect tool’
BMI is a crude measure of the percentage of body fat people have. “BMI ignores the thing that’s really important [in causing diseases], which is fat mass,” says John Cawley, professor at Cornell University and author of a review on BMI and alternate measures of fatness published in the Journal of Health Economics. Since it doesn’t distinguish between weight from fat and weight from muscle or bone, BMI isn’t very accurate at judging how much body fat people have – which is the key issue when it comes to preventing weight-influenced diseases such as diabetes, heart disease and cancer.
As Travis Saunders knew, as a result BMI sometimes wrongly characterises very fit people as overweight. Bodybuilders and athletes can even fall into the obese category. More concerning, many people with a normal BMI actually have too much body fat. A 2008 study in the International Journal of Obesity found that calculating obesity with BMI missed fully half of the people who were obese as measured by body fat percentage. “There are people who don’t meet the BMI criteria for obesity but certainly have weight related health problems,” says Arya Sharma, Alberta Health Services Chair in Obesity Research and Management at the University of Alberta.
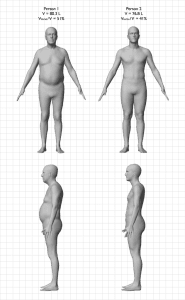 The potential difference in body fat percentage is shown in this image, which shows two men who have identical BMIs of 25.5, but very different body shapes thanks to differences in how much of their weight comes from muscle and bone (image courtesy of Body Labs).
The potential difference in body fat percentage is shown in this image, which shows two men who have identical BMIs of 25.5, but very different body shapes thanks to differences in how much of their weight comes from muscle and bone (image courtesy of Body Labs).
BMI also works less well in certain groups, including men, who have less body fat than women. A 2013 meta analysis found that for the elderly, BMIs over 23 might be healthier. As the Canadian guidelines explain, BMI also has limitations when it comes to non-Caucasians, with research suggesting that Asians should possibly be classified as overweight and obese at lower BMI ranges, and black people overweight and obese at higher ones.
Where you carry your weight matters, with belly fat being the most likely to result in diabetes – even in people at a healthy BMI – and heart disease. Carrying fat on your hips and thighs, on the other hand, is less harmful and may even protect you from diabetes.
Those caveats are why BMI should be only one of the ways doctors assess patients. says Brauer. “BMI is an imperfect tool, but it’s not the only tool that physicians have. A physician would never be only talking about BMI – they would always be looking at the whole person.”
But the worry is that, in fact, they will be giving it unfair influence, says Freedhoff. “You’ll end up making errors on both sides. You’ll potentially ascribe healthy lifestyles to people who are thin, and unhealthy lifestyles to patients who could be living incredibly healthful lives… Ultimately, I’m not a fan of BMI as a clinical tool.”
“BMI is not very helpful,” agrees Sharma. ““There is very little relationship between BMI and health except that the probability of having a health problem gets greater as BMI rises. But at every level of BMI there are people who are healthy and people who are unhealthy.”
Weight loss difficulties
Another part of the issue is that offering counselling on weight loss may not be helpful. “There’s not a lot of evidence showing that if you discuss BMI with a patient it’s going to make a lot of difference,” says Sharma.
That’s because losing weight is so difficult. “If you had a simple and easy treatment [for weight loss] that actually worked, you would recommend the treatment,” says Sharma. The problem is, we don’t. “You’re lucky if you can get a 3% weight loss sustained over two years [through diet and exercise].”
“Physicians wrongly assume that this is a very straightforward issue: eat less, exercise more. Forks and feet,” says Freedhoff. “But the same doctors likely would not assume that people with depression should just cheer up. I think those are comparable.”
Alternates to BMI
Sharma has developed an alternate ranking for obesity, the Edmonton Obesity Staging System. Intended to be used alongside BMI, it classifies patients by physical symptoms, such as diabetes or heart failure; psychological ones, like depression; and functional limitations, like reduced mobility.
Another common alternative is waist circumference. Since having a larger waist increases the risk of type 2 diabetes and cardiovascular disease, where you carry the weight is important. Waist circumference strongly correlates to body fat percentages, and along with BMI, it’s currently used to screen for type 2 diabetes in Canadian adults. Health Canada recommends using both waist circumference and BMI, saying men should have a waist of less than 40 inches, and women of less than 35 inches. Waist-to-hip ratio is another option, since it’s also predictive of diabetes and cardiovascular disease.
Some high tech options also exist, including underwater weighing and Dual Energy X-ray Absorptiometry, which uses low levels of X-rays and is considered the gold standard in measuring body fat. But they tend to be used only in research. That’s because they’re more expensive and time-consuming, and work less well in the very obese.
In the end, which measurement is best may depend on what you’re looking for. “If you’re trying to predict heart attacks, waist circumference is best,” says Crawley. “For diabetes, it’s measuring fat mass. If you’re looking at arthritis, maybe BMI is fine.”
Or maybe it’s not worth focusing on the measurements at all. Lifestyle changes like exercising more “have impacts on cancer, mood disturbances, sleep apnea, chronic pain … the list goes on and on and on,” says Freedhoff. “As a society and as a profession, we tend to only talk about lifestyle in the context of the scale. But if everybody can benefit from improving their lifestyle, that’s where the focus ought to be.”


The comments section is closed.
I learned relationship between BMI and health except that the probability of having a health problem gets greater as BMI rises. But at every level of BMI there are people who are healthy and people who are unhealthy.
I’m 6’1″ and 220 lbs with a 33 inch waist. I can see my abs. I have 18.5 inch muscular biceps. Accordign tot he BMO I’m obese. The BMI is a joke.
Some Health Centres who work with pre-school children would like the nurses to refer children with a BMI over 85% to their physician for weight management follow-up. The message parents are given is that a BMI of 85% means that the pre-school child is at risk for being overweight later in life.
Many parents tell us that their child eats a healthy diet and is active on a daily basis. They question the validity of the presupposition that a higher BMI in a child can predict weight in the future.
Again, should we use the BMI in pre-school children as a talking point for healthy eating and active lifestyle? Must we rely on the BMI?
Should we use BMI for children?
That’s a great question Lois – at my 11 yo’s last appointment, she was in the low normal BMI range and the doctor commented that she should watch what’s she’s eating and exercise more. She’s a gymnasts – spends 4 evenings a week working out and has abs most adults would kill for. But apparently, they take the BMI and then plot it on a percentile scale and because she’s heavier than most kids her age and height (and much more muscular too), she was deemed overweight. I was VERY disappointed with the doctor. I’m of the opinion that they should not. A clear look at her would have made it clear she wasn’t overweight. Way to take that pre-teen kid and make her self conscious about her non existent weight problem.
I understand your dilemna. Athletes are often wrongly assessed to be ‘overweight’ when, in fact, they are from it.
A certain very well-known Hollywood star, famous for his muscles and many action movies, was deemed to be ‘morbidly obese’ – there was not one ounce of fat on him!
As medical professionals, we need to be careful how we approach the issue of weight with parents and children. Basing our assessment and messaging on the BMI makes little sense when the child is healthy, eating appropriately from all food groups, and active.