By all accounts, Kaiser Permanente (a non-profit healthcare insurer and provider in the United States) is one of the best performing health care systems in the world. Shouldn’t it follow then, that its health plan members fare better as a population in terms of their health status? Not quite.
A few weeks ago, Kaiser Permanente was in Toronto to share their approach to health promotion and illness prevention. We often look to leading health systems like Kaiser Permanente for inspiration, as they are years ahead of Canada in putting in place major innovations in their health care system, for example:
– A fully integrated electronic health record for all 9 million plan members and their care providers actively use across several US states, as well as a personal health record that more than 60% of its members voluntarily access and use
– More than 40% of primary care consultations occur via phone, e-mail or video consult, and rarely does a patient see their physician to receive a prescription.
– All physicians are on salary, with a highly transparent performance management system that proactively alerts providers to gaps in their patients’ care profiles, and rank orders physicians against their peers against several key indicators
Indeed, across the 39 health care delivery indicators set out by a national healthcare quality council in the U.S.A., Kaiser Permanente’s health system is among the best performers, and is in 1st place for 11 of the 39 indicators.
If I were to ask whether Kaiser Permanente patients have superior health “outcomes”, the answer would be a resounding yes. This is precisely what is reflected in those 39 quality indicators where Kaiser Permanente is a national leader. Lower hospitalization rates. Fewer hospital re-admissions. Better medication adherence. Earlier cancer screening and diagnosis. Fewer unnecessary tests. That is, if you are a recipient of Kaiser Permanente’s health care services, you will have a superior experience and better clinical outcomes for less cost than most other health systems.
Yet despite the excellent medical care delivered by Kaiser, their members as a population are not necessarily any healthier than the non-Kaiser population, or even the uninsured population.
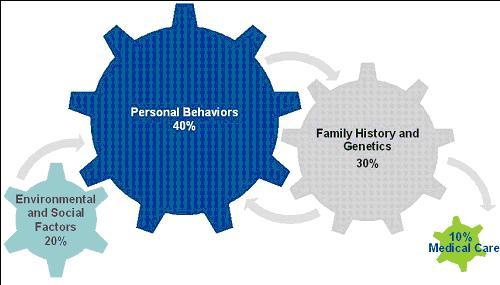
There were two key slides in their presentation that explained why this is so. The first was their up-front acknowledgement that only ~10% of population health is driven by the medical care that one receives (socioeconomic, environmental, behavioral and genetic factors making up the remaining 90%):
Source: McGinnis et al, Health Affairs (2002)
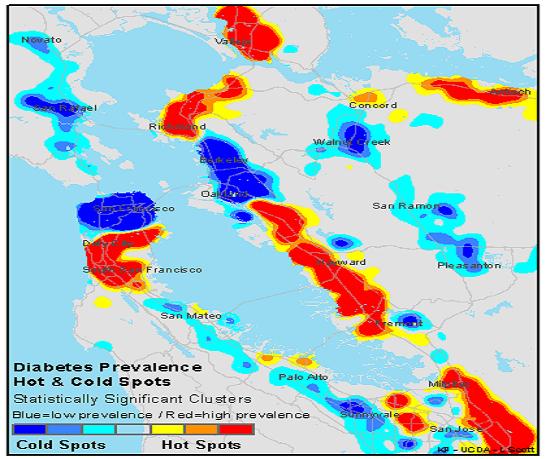
The second was their validation of this theory with empirical data. They presented a series of charts showing the geographic distribution of the incidence of risk factors for disease (obesity, hypertension) as well as disease (diabetes) amongst plan members in a state. This one is shows the diabetes “hot spots” and “cold spots” by geography:
Two regions adjacent to each other displayed diametrically opposite rates of diabetes. So what was the difference between these? It wasn’t the quality of the health care system they were accessing – these maps show only Kaiser Permanente patients – patients in these two areas access the exact same high quality health care, at the same facilities, with the same robust tools and technologies that Ontario is currently investing heavily to put into place. Yet one population is healthy and the other is not. So what was the difference? Socioeconomic status within the geographies that the different populations reside. The same holds true for obesity and hypertension. In each case, the “hottest” spots for these modifiable risk factors are in lower socioeconomic status areas, while the “coldest” spots are in higher socioeconomic status areas.
What this means is that place shapes disease. Medical care can do very little to affect this reality. That is why Kaiser aggressively invests up to $2B of its $46B budget (yes, roughly the same budget as Ontario’s public health system) into upstream health promotion and social capital. And they will admit that they are barely making a dent – as a health care insurance and delivery system, there is only so much they can do.
Before Ontario goes down a path of attempting major, highly difficult, structural and financial reforms, can we learn from the sobering lesson of Kaiser (who has already been there, done that) and divert as much economic investment as possible – at the Ontario program spend level – into upstream health and promotion? After all, is the goal of our health system to be “a high performing” system? Or is it to improve public health?


The comments section is closed.
Very interesting read. Re-enforces what we know but really provides a nice graphical way to drive the point home. I really liked the reply by Reghu Kurian, and am left with a question:
Is poor health outcomes a consequence of consumerism?
This is an excellant presentation Zayna. As a physician this is not new to me. Prevention is always the key in reducing prevelance. Now how to reduce the Chronic diseases when genetics and family history play a role??? A million $ question. I read an article recently about can government dictate what you eat? This all boil down to the human behaviour to food, exercise and finding a partner. Agree with Catherine, (Sorry, not to offend anyone, but if you need your children to be healthy, your partner selected should be from a healthy background-genetically). Now if you cant do anything about genetics, then you can do some thing about preventing diseases by healthy eating, exercising, not smoking, and other high risk behaviours like drunken driving, bungee jumping etc. We as healthcare system is a disease treating organization; not one preventing. So why cant we do it easy way? Advertise the reason for diseases every where including every time a TV advertizing about junk food appears? I am surprised that we are spending billions to make a 10% dent in the population? Economically it doesnt make any sense!
This is an excellent point, Zayna, and very well articulated. You may want to also see a recent TED talk by Rebecca Onie (founder of Health Leads). Her program tackles some of the socio-economic determinants of health, including access to basic resources.
Thank you, and all the best.
good health starts very early — prenatal, in that the habits of the parents will determine those of the children. Some evidence suggest this starts at a genetic level, not just post-birth behaviour. This is not a health budget issue but one for the general revenues of a province/jurisdiction and yes, poverty is determinative
Very interesting post Zayna. Excellent observations about measures and how little they actually relate to what matters to people. Are you aware of the work of Prof John Seddon? I think it might be of interest to you. His is a method that looks outside in from a users perspective. You can find out a bit more here if you are interested http://www.thesystemsthinkingreview.co.uk/. We are relative newcomers in health so learning all the time, but here is a link to an example what we are finding as a result of our studies in health http://vanguardinhealth.blogspot.co.uk/2012/02/plan-b.html. Understanding people in the context of how they live their life, developing and tending to relationships end-to-end over time rather than the relentless pursuit of efficiency is better it seems.
Well done.
A good reminder that having a high performing health care system is necessary but remains the smallest overall contributor to improving public health.
Similarly, a great deal of effort will be required to discern the combination of specific socioeconomic, environmental, behavioral and genetic factors that make the greatest contribution to improving public health.
Our challenge collectively will be in establishing the necessary evaluation tools to refine our understanding, establish public and professional education and enabling policies, regulations and structures to allow for the greatest improvement in health for the largest number of people possible.
The best, clearest, most publicly accessible description of something I have always struggled to adequately express. Thank you.