When talking with my family and friends outside of healthcare I get mixed reactions to what eHealth means. Responses can range from simple to sad.
“Is that like MRIs and stuff?
“Do we have electronic records like at the store?”
“My doctor has a Blackberry…. but I can’t email him, so I don’t know.”
However, after further discovery I find out many of my friends have some sort of electronic device that makes their health better. I just have to open Facebook[i] to see who is going for a run with their Nike+[ii] shoes, or Foursquare[iii] to see who might be visiting a gym. I can log into PatientsLikeMe[iv] and find others tracking their illness and collectively learning about how to be healthy.
Consumer focused solutions are some of the most exciting changes in eHealth. They shape the way we think of health. Through out nursing school I was presented with a few definitions, but more recently I’ve come to use Huber et al (2011) proposed definition:
Health is the ability to adapt and self manage[v]
This definition speaks to me because it is about what an individual can do to improve their own health, but I’d take it a step further. Caregivers also need to be able to part of the adaptation and management of the changes to the individual to empower and support individuals that may not have the resources or lack the personal capacity to be fully independent.
This idea of health as self management, when paired with the consumerization of healthcare products, is exciting. During early development, new technology is often cost prohibitive, but prices slowly come down as production methods improve. Now apply this to healthcare, in the past the ability to take an ECG required an expensive machine.
Blood pressure cuffs were something you’d only see in a hospital, pharmacy or your family doctor’s office. Now both of these devices are reasonably affordable, and not only that but they allow you to track and monitor your own health. Many of them even give you feedback to help you improve your health.
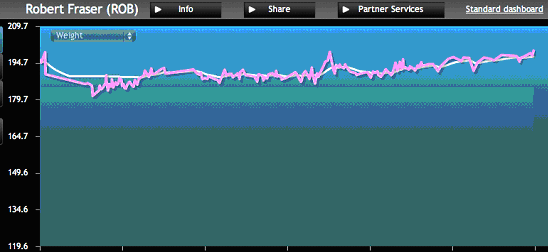
What excited me about this is how it makes eHealth increasingly accessible for those interested in monitoring and improving their health. Many of these platforms, such as PatientsLikeMe are free, giving anyone with an internet connection access to these services. And the continual monitoring is also important, because one number is easy to dismiss, where as continual reminders, prompt tips, and trend lines are much more engaging and harder to ignore. Personally, I had to struggle with this as realization as I slowly saw my WiThings[vi] scale flutter up and down enough for me to dismiss it as water weight, or just one bad weekend. However, once I saw the trendline, the truth sank in. It was unfortunately and undeniably going up and to the right.
Not only do these technologies engage the user in their own health, but they also provide a community and a social activity. For example, I can share my weight and blood pressure from WiThings with friends and family members. Flip this around and I could keep an eye on my father’s blood pressure and weight and check in on him if I notice any changes in his health.
Other devices like Nike+ or the EndoGoddess[vii] create games and challenges or reward users for monitoring their health. The EndoGoddess app gives diabetics iTunes rewards so children can download a song if they enter their blood sugar scores a certain number of times. How exactly is that social? Well the app is not a social network like facebook, but it has a built-in social component. When users sign up, they can send out a request for support from their friends and family. The request actually collects small amounts of money that will be used to buy iTunes credits that are used as an incentive to the diabetic user. As they successfully learn to monitor their blood glucose and make healthy decisions they are given rewards and the ability purchase songs or games. I find these particularly fascinating because others are more engaged and involved in promoting and supporting others health goals. Your friends don’t have to be health experts, but they are given some teaching and explanation of why these behaviours are important and invites them to support and encourage you in your healthy behvaiour.
Unfortunately at this point there are few healthcare organizations that are capturing data from these non-traditional sources for use in the traditional healthcare settings. In the future, I hope this trend will change. Why not recommend patients explore the kidney transplant group? Especially since our organizations are not currently offering any equivalent or similar service. These tools can provide valuable social support, and if we engage with them they can be useful tools to help us collect better health data to understand illness. More importantly, they help individuals feel empowered and that their actions can meaningfully improve their understanding and ability to adapt and live with their illness. That is powerful and exciting, which is why anyone asks what I’m excited about in eHealth I end up talking about mobile phones more than Electronic Health Records.
Rob Fraser is not associated with any of the products or companies referenced in this article.
[i] Facebook is the world’s most popular online social network.
[ii] Nike+ is an online platform that collects and tracks user’s running activity that is collected from manufacturer’s devices (podemeter, GPS watch, heart rate monitor, mobile apps, etc.)
[iii] Foursquare is a location based mobile application that allows users to check in at places they are visiting.
[iv] PatientsLikeMe is a platform for patients, researchers and healthcare providers that allows users to input and track health related metrics (blood serum levels, mood, feeling, drug therapy levels, etc.) and share their information with an online community that has the same illness
[v] Huber, M., Knottnerus, J. A., Green, L., Horst, H. V. D., Jadad, A. R., Kromhout, D., Leonard, B., et al. (2011). How should we define health? British Medical Journal, 343(jul26 2), d4163-d4163. doi:10.1136/bmj.d4163
[vi] WiThings creates wirelessly connected healthcare monitoring devices such as weight scales, blood pressure cuffs, and baby monitors. That can be wireless connected to store and share data.
[vii] EndoGoddess App allows users to store and monitor blood glucose levels and provides rewards for entering data such as free iTunes music downloads that are purchased by their social network.


The comments section is closed.
Hi Robert, thanks for your response. I am not suggesting anything you wrote is unreasonable. My commentary is less that of saying you are wrong (because you are not), but rather, that there is another perspective that is critical to the discourse on eHealth/mHealth. In its most simple formulation: the public interest – who, what, why and how?
Health care has always been subject of innovation and diffusion, most frequently driven at the micro level of creation and practice by entrepreneurs and early adopters. The ‘micro’ drives dissemination – but if left to independent forces alone it establishes the ‘macro’ by default. Not sure that we want that. Hence my widening the perspective to issues of the macro. Markets and individuals are critical to driving change, yet past experience, which is still relevant, suggests these forces lead to positive, negative and unintended consequences. History tells us ineffective and inefficient practices can rapidly fill the health system and become incredibly difficult to alter or remove once entrenched. Indeed, our fragmented health system reflects a historical pattern of the micro forming the macro. So why not establish a systematic macro perspective on eHealth/mHealth at the outset and avoid the policy failures of the past?
Thanks for the link to Will Falk’s recent article. Not sure why I missed this and I am clearly trespassing on some of what he wrote – except he wrote it better. (I did have to chuckle he also uses the term “wild west”). In particular, I like his conceptual distinction of “TechRx” and “Apps Pharmacy”; an extremely useful categorization for discussion, research and action. However, it is primarily focused on elements of the “what” question, while I think we need to take it back to the base roots: who the heck is going to assume some leadership?
Policy innovation is quite simply the idea of new ways of generating, organizing and regulating public policy.
Currently, there are organizations such as Health Canada, the Canadian Agency for Drugs and Technologies in Health and provincial Ontario Health Technology Advisory Committee, as well as researcher/clinician initiatives such as the Programs for Assessment of Technology in Health (PATH) Research Institute. Their current mandates and design regarding safety, effectiveness and cost effectiveness are not well aligned with the emergence of new categories of “health intervention”. Policy innovation asks the question: are these the appropriate organizations and forms of process to deal with the new world?
Is it simply a matter of creating a new department or are there other ways? Will a bureaucratic approach or some system of ‘command and control’ provide the speed and flexibility to such a rapidly changing world? Probably not, so then what? Is there a place for social enterprise? Anecdotes, case studies and process studies help articulate the early waves of innovation, but the bottom line still needs to be clarified and affirmed by randomized controlled studies or empirically valid quasi-scientific methods. How well are existing evidence based knowledge development and knowledge transfer organizations adapting to the emerging digital world of health?
Current micro dissemination, uptake and utilization are driven by market forces and the bulk of “knowledge” emanates from these sources. Do we really want to make the eHealth/mHealth INDUSTRY the ‘de facto’ knowledge transfer agency? Even younger health providers who are generationally more comfortable and savvy with digital devices are essentially experienced “amateurs”. Is the policy ethos to be “just do it”? Should the key source of knowledge come from industry sponsored or influenced conferences and learning symposiums? Is the scattered uneven work of public sector institutions or bright individuals sufficient to create a reliable system of knowledge transfer? There is a clear need for constructing professional standards in eHealth/mHealth aligned with curriculum development and other forms of public professional development to take providers from the world of amateur to professional.
So you reflect well the enthusiastic leadership of early adoption at the individual, micro level; a totally necessary stage of evolution. There exists resistance and delay in many parts of the health care system, but I would suggest we are reaching the now cliché “tipping point”. Once that initial resistance falls then the system will no doubt be overwhelmed by new devices, apps and programs. If we don’t now start building the structure and process of evidence based eHealth/mHealth with checks and balances, the future will be driven by the micro and too often shaped by untested technologies and approaches. Thus, my commentary was a call for balance with a macro public sector response.
Fantastic article, so much of it rings true.
We need to figure out how to incorporate so much of what is now possible (e.g. continuous monitoring, incorporation of social networks) into the formal health system.
I think a simple step would be to spread awareness of what’s out there and have them pass it on.
Thanks personally for the tip on Patients Like Me.
Cheers.
Here are some links to some interesting reports on the emerging world of mHealth
The effectiveness of M-health technologies for improving health and health services: a systematic review protocol http://www.biomedcentral.com/1756-0500/3/250
• Contains a useful conceptual framework for classifying mHealth tools
Getting to Value: Eleven Chronic Disease Technologies to Watch, NEHI, June 2012
http://www.nehi.net/publications/72/getting_to_value_eleven_chronic_disease_technologies_to_watch
Booting Up Mobile Health: From Medical Mainframe to Distributed Intelligence Report (Health Horizons Program, Institute for the Future), 2009
http://www.iftf.org/node/2810
The future impact of digital technology on health behaviour, health status and the health system is marked with keen anticipation. Yet there remain significant questions. Not only questions of effectiveness, but also potential unintended consequences and harmful side effects. While I share some of your enthusiasm, I carry along with me a concern that there has been little in the way of concerted and coordinated action by regulatory and policy sectors to define the public health interest in what is currently a wild west of innovation and invention.
Your article contains a host of relatively untested statements and assumptions. For example, “More importantly, they help individuals feel empowered and that their actions can meaningfully improve their understanding and ability to adapt and live with their illness.” Well, that’s the theory – what is the evidence? There are speckles of research, but the findings are mixed and unsystematic. Similarly, “I can share my weight and blood pressure from WiThings with friends and family members. Flip this around and I could keep an eye on my father’s blood pressure and weight and check in on him if I notice any changes in his health.” Yes, but that leaves unanswered at what point does self monitoring slip over the line of health to unhealthy (after all, one can legitimately ask if constant monitoring of vital signs and personal health indicators is less about positive health behaviour, awareness and control and more about obsessive compulsive behaviour). And while we could say leave it to the individual, there is a strong likelihood such compulsive behaviour will trigger utilization of the health system – so there even on the narrowest criterion there is a public interest to be defined.
Which leads me to my main point, how are public authorities responding? Not at all might be an over-statement yet not far from the truth. With every new ehealth/mhealth innovation, new questions are generated. However, the answering of these questions is scattered among various academics/researchers or simply not being addressed. Mhealth devices are creating a grey area that must be defined. Are these simply products like the “Ab Pavelizer” or are these medical devices requiring significant health regulation? This becomes especially important if devices are being utilized in the context of a regulated health professional and/or setting. But without a locus of accountability and process of scrutiny – establishing parameters, creating regulations and standards, and monitoring and enforcing compliance – such a question is neither being asked nor answered.
So I am not arguing we quell the enthusiasm of the potential which you capture so well, or trying to play the role of Luddite. Instead, I am suggesting that while the motive of profit will easily provide the impetus for unbridled innovation, there is an urgent need for a wave of enthusiasm to initiate a process of defining the public interest – matching technological innovation with policy innovation.
Appreciate the thoughtful comment Ron!
Thanks you for calling out some important points. A lot of this is breaking ground, and it is very new. I took a bit of liberty, since this is our Opinions section, but I don’t think I said anything unreasonable.
So if I can, can I ask your opinion? What exactly is “policy innovation” and how would it help? I’m no expert on what pragmatic regulation and/or policy would look or where it would be most appropriate, despite understanding it will be critical.
Getting the policy and regulation right is crucial. Something that I worry about us getting wrong. My perspective is, less is more and only where most appropriate. Will Falk wrote a great Opinions piece about how Apps will be prescribed and adds an excellent perspective to this conversation [http://bit.ly/Qf3UBQ]. It does not advocate for cumbersome regulation across the board. However, when an application for an digital tool is clinically prescribed or part of organizational/systematic as a potential cure it is critical to have the right controls and evidence. The rest he relates to the vitamin and health food markets. In that industry we place some restrictions, monitor quality, and prevent/regulate unsubstantiated claims. Why not follow this example?
I hope that the “wild west” as you and Mr Falk call it, continues to innovate and push our understanding of what is technically possible. PatientsLikeMe did not begin with evidence, and fortunately were not restricted by regulation. The community started with a focus on what was possible. Now that they want to be taken seriously by healthcare providers, organizations and pharmaceutical companies they are developing the research evidence. This is where the data begins to improve our insight and support or weaken the original opinions.
You asked about the evidence for empowerment and life style modification. Research on online communities like PatientsLIkeMe has found users gained greater understanding of their illness, changed their behaviour and in another study reduced risky sexual activity[1]. “Users gained a better understanding of their seizures (58%), learned more about a symptom or treatment (55%), felt greater control over their condition (50%), had reduced side effects (27%), improved adherence (27%), and had insisted on seeing a specialist (17%) or, in some cases, even changed their physician (10%).” [2] I agree that the evidence is not as substantive as we would like, and other communities have varied results.
As the literature grows we will better understand the nuances. Perhaps, those statistics are biased by the site, or perhaps they have the right formula for their community, and not all online communities will be effective. Only time and more data will tell. And this is why I think this area is so exciting.
The other point I wanted to address is the potential harm of these web services and apps. Targeting certain metrics may lead to over emphasis of certain measure. This is why I think the definition of health I mentioned is so important. Health is not just the absence of disease or hitting a certain recommended range. It is the ability to adapt and self-manage. The ability to understand how to modify activities to accomplish goals. The running system has not fixed my weight, but it does give me a greater sense of control and understanding of how I can improve my fitness and increase my sense of control. Do we not need to give our patients these a sense of control over their health and the ability to affect their illness if possible?
The other aspect of risk you mention are the possible negative side effects. Traditional western medicine, falls into both categories of risk, focusing on particular indicators (metrics) of illness, and treatment comes with consequence (risks, outcomes, side effects, etc.). This is causing some concern about over-diagnosis and over-treatment that may be harming patients [3]. My hope is not that apps replace traditional medicine. Instead it can supplement and enhance our current methods of treatment and the way our system works.
Apps can create new capacities for healthcare, and enhance activities we already do. We often lament our “illness system” that only treats disease. Digital tools create new potential, but yes they will come with risk. Everything has consequences. Even drinking too much water can be harmful. I do not think risk is a bad thing, but it ALWAYS needs to be balanced by potential benefit and/or harm. I agree with you, enthusiasm needs to be matched caution.
Really what I hoped for from this article is that it might ignite others curiosity about consumer health innovations. A curiosity that should be paired with healthy doses of skepticism and a lot critical thinking.
Thanks again for the thoughts, and the great articles!
Rob
[1]Wicks, P., Massagli, M., Frost, J., Brownstein, C., Okun, S., Vaughan, T., Bradley, R., et al. (2010). Sharing health data for better outcomes on PatientsLikeMe. Journal of medical Internet research, 12(2), e19. doi:10.2196/jmir.1549
[2]Wicks, P., Keininger, D. L., Massagli, M. P., de la Loge, C., Brownstein, C., Isojärvi, J., & Heywood, J. (2012). Perceived benefits of sharing health data between people with epilepsy on an online platform. Epilepsy & behavior : E&B, 23(1), 16-23. Elsevier Inc. doi:10.1016/j.yebeh.2011.09.026
[3]Moynihan, R., Doust, J., & Henry, D. (2012). Preventing overdiagnosis: how to stop harming the healthy. Bmj, 344(may28 4), e3502-e3502. doi:10.1136/bmj.e3502
Super duper article, Rob!
The possibilities are endless indeed and the e-health applications will only grow with time. It amazes me how much information and resources we have already available that can help us to track and improve our health, individually and as a community.
I never really thought of e-health in this context. Thanks for giving me and others much to think about and to possibly embrace for our own good. Health awareness, education and adoption of new technologies and discovering new ways to be a more engaged patient and/or caregiver all factor into enhancing our overall health and well-being and that of our loved ones. For every e-patient, each aspect of e-health has the potential to be quite empowering.
All the best!
Catherine Richards
PS I still think we need electronic health records made available and accessible to every e-patient in real time. I also think e-patients and/or substitute decision makers should own the rights to their health information instead of, for instance, a long term care home retaining a resident’s original health records for 50 years after a person’s death. The MOHLTC too seems more interested in holding on to its formidable power regarding patients’ (and substitute decision makers’) access to health records of all types and from my experience much of the power over our health and our health records is in the wrong hands. I would prefer to accept responsibility and take ownership of my own health and health records in partnership only with those I trust and choose to involve.
Thanks Catherine!
I agree there are a lot of other important parts of eHealth that we need to keep pushing forward on! From functionality to patient awareness! There is definitely no shortage of work to be done.
Hopefully we all can continue to look at what is happening on the periphery and consider how it might be explored, researched, and integrated into a system that focuses on improving people’s health.
Appreciate the comment!
Rob
Thanks for the feedback, Rob! I agree with you and I plan to continue as you suggest exploring e-health as more broadly defined by you . . .and with an open mind!:)
Keep writing – I look forward to hearing more opinions from your perspective in the future!
Catherine