When provincial and territorial Health Ministers meet Wednesday with the new federal Health Minister Dr. Jane Philpott, it is imperative they focus not simply on the amount of money coming from Ottawa but rather on what matters most: how to get value and performance from our health care dollar.
The late Jim Flaherty set the table for the upcoming discussions in 2011 by announcing that growth in federal funding to health care would be slowed. In many ways, a challenge was handed to the provinces and territories to deal with their own inefficiencies, and some progress has been made on that front. Acting without the federal government, the premiers’ council of the federation has made some progress in advancing a pan Canadian pharmaceutical alliance (pCPA). While the pCPA is still evolving, this structure offers hope of moving Canada from its place as a “price taker” – Canada is one of the highest per capita pharmaceutical spenders – to a “price maker.” Rather than each province and territory negotiating deals with pharmaceutical companies for government-covered drugs, the pCPA allows for one nation-wide bargaining team, and bulk purchasing of drugs. Perhaps achieving better value in healthcare spending is possible.
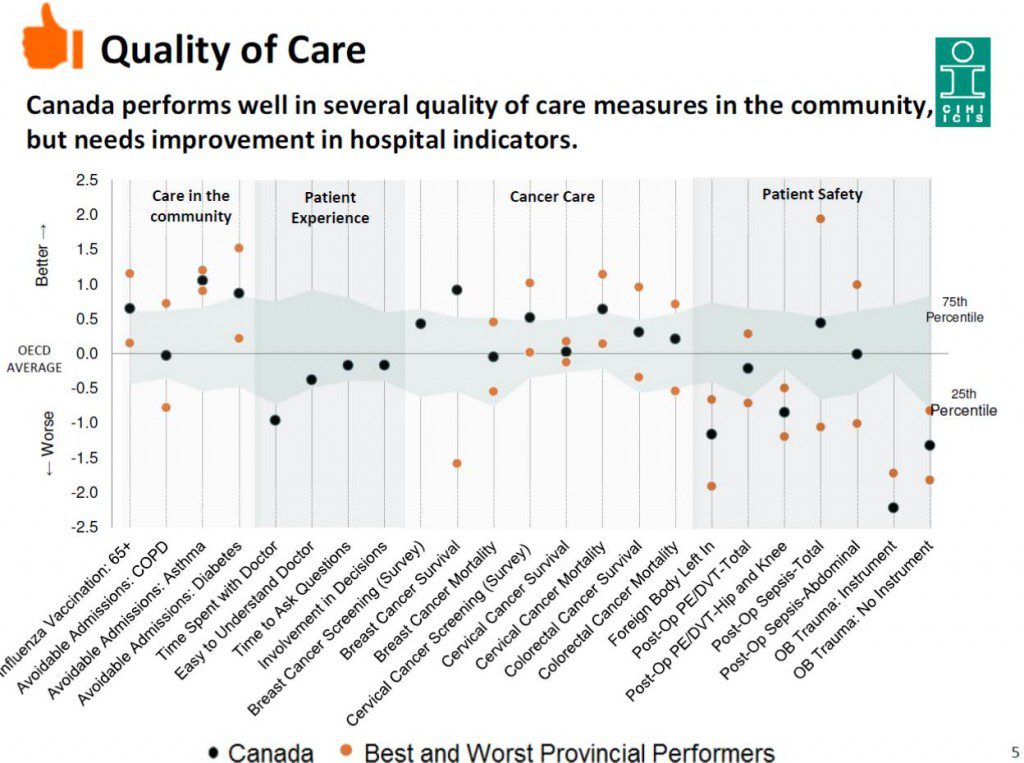
The OECD’s 2015 report on health care spending and performance around the world does not flatter Canada with respect to quality, value and performance. Canada does not compare particularly well in quality of care, with a few notable exceptions – cancer treatment and cardiovascular care – while patient safety remains an issue, despite our relatively high spending. Even though important gains have been made on wait times for hip and knee replacements and cataracts, we remain far behind the pack when it comes to wait times for access to primary care and specialists. We are hardly doing better than the OECD average on indicators of mortality from suicide, heart attacks, and transportation accidents. And still over 10% of the adult population cannot get access to needed drugs because of financial barriers. When we break down these results at the provincial and territorial level, results are especially concerning in certain parts of our country. Simply put, the progress in the value, quality and performance of our health services in the last ten years has been modest, with the exception of a few areas that were targeted in 2004 with investments.
In the federal Health minister’s mandate letter, the newly elected federal government called for a multiyear Health Accord with Canadian provinces and insisted that the government should be transparent and focused on results. To achieve this, a new Health Accord should focus on reporting measures that are vital in understanding a health care system’s performance. Currently, provinces report very few patient reported outcome measures and few patient reported experience measures. Information that can be compared across provinces must be collected and reported transparently and should be put to use to support decision-making, research, and to inform Canadians about the value they get from their health care system.
Examples of indicators which should structure the next Health Accord include:
- wait times to see a GP
- wait times to see a specialist
- amenable mortality (defined by the OECD as “premature deaths that should not occur in the presence of effective and timely care”)
- the percentage of the adult population not getting access to necessary drugs because of financial barriers
- patient safety measures like surgical complications
- patient reported outcome measures for select interventions
- patient reported experience measures for select interventions
Simple provincial targets can be established for each measure, taking international evidence into consideration. Each province should define how it intends to achieve its targets and how this effort will gradually reduce wide inter-provincial performance variations.
With a new federal government in place and ready to engage, there is an opportunity to shift the accountability relationship to what matters most: improved health outcomes and value for money. It may be too challenging to link federal funding to how well the provinces perform on these indicators given their different geographies and capacity. However, the provinces should be bound by any agreement on transfers to work in a public and transparent way to improve these indicators in a common public format, optimally through the Canadian Institute for Health Information, our federal-provincial health data reporting organization. In this way, providers and consumers will be able to point to areas where their provincial health system needs improvement, target these areas for priority effort and report on their successive improvements.
The evidence is clear that public reporting improves the quality of health care. Working towards specific target areas, Health Ministers can set a new bar moving forward in 2016 with evolving targets in the area of value, quality and performance.


The comments section is closed.
One reason that Cardiovascular and Cancer Care are doing so well is because in each there is a REAL system in place that requires accountability and transparency. Public reporting is an important tool but it must be timely and audited. I’ve seen too many examples of false or wishful thinking public reports. It is important to eliminate blame and shame but to encourage continuous improvement in results and outcomes. Canada has been among the ‘top’ spenders (except for the USA) for a long time. Our poor value for money is a serious issue! I also completely agree with Dennis Kendel. (see below).
As a member of the former Health Council of Canada, I support the call for public reporting on the quality of healthcare across Canada. Such public reporting might serve concurrent accountability and quality improvement goals. I would strongly favor reporting that is designed to foster quality improvement as accountability reporting tends to foster distrust and gaming. If there is to be another Accord or some other form of FPT Agreement, it must be one that is forged and embraced by all FPT governments. I’d also like to see the existing Health Quality Councils become more actively engaged in inter-jurisdictional QI collaboration so we can learn more effectively from one another across the country.