Modern medicine has had a wonderful impact on society in the past 50 years but recent events have illustrated that healthcare can do harm as well as good.
Take, for example, U.S. President Donald Trump in May touting hydroxychloroquine, a malaria drug, as a “game changer” ready for immediate use for treatment of COVID-19 and claiming to be taking it himself.
Decisions about the safety and effectiveness of drugs are based almost entirely on what is known as a randomized controlled trial (RCT) in which patients are randomly assigned to receive a treatment or not. Since May, RCTs on the effectiveness of hydroxychloroquine in the treatment of COVID-19 have reported that it produces little or no reduction in the mortality of hospitalized COVID-19 patients when compared to patients who received standard care. It is certainly not the hoped for “miracle cure.”
The situation with hydroxychloroquine highlights the importance of being sceptical of “miracle drugs” such as those advertised on TV and knowing there are risks associated with every medication. This is especially important for people with underlying health conditions (heart disease and stroke, diabetes, long-term lung disease and cancer) who are at increased risk of COVID-19. As well, the more underlying conditions individuals have, the greater the risk of both COVID-19 and polypharmacy.
Polypharmacy is the concurrent use of multiple medications. On average, people over the age of 65 are on six drugs a day. Often the physicians who prescribe the drugs do not communicate with each other, which can result in a patient getting drugs from each of their specialists, like their cardiologist, neurologist, psychiatrist and endocrinologist. Polypharmacy increases the risk of heart disease, atrial fibrillation, high blood pressure, diabetes, long-term lung disease and delirium. Patients, with the assistance of friends, family and healthcare practitioners, need to assess the following:
- Are the drugs you are taking incompatible when taken together?
- Are you able to easily obtain your drugs in your community?
- Are there reasons why you are not taking the medications?
- Are you keeping track of how you are doing while you are taking your medications?
Rather than looking for another pill to cure your next ailment, look in your community for other approaches to improving your health and quality of life. Pain control is a good example of the importance of non-drug approaches to ailments and can eliminate the risk of addiction to pain management drugs that people experience. For example, pain can be decreased and stress relieved with relaxation techniques, such as:
An important fact is that people most at risk may be the ones least able to ask for reviews of their medications. Physicians have a responsibility to de-prescribe drugs after reviewing medications for people with multiple prescribed drugs to stop or decrease side effect risks and improve outcomes. If patients are concerned they have been prescribed multiple medications by different physicians, they should ask their family physician for a full review.
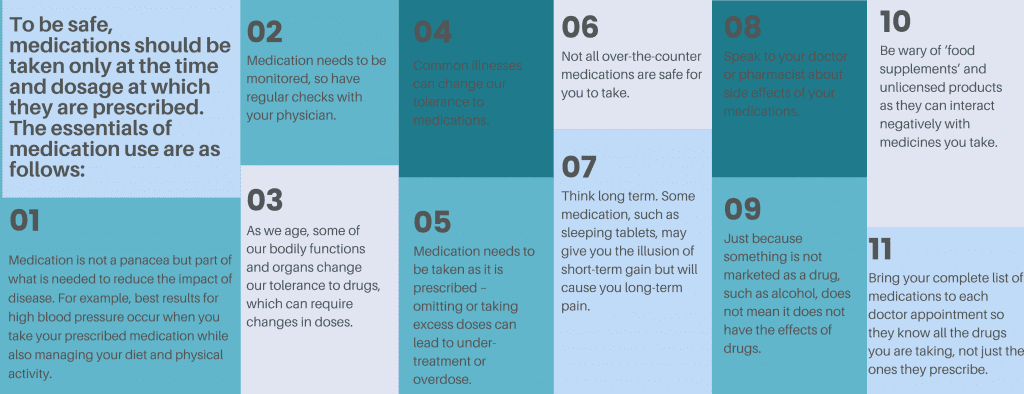
Everyone should check with their doctor before mixing medicines, including over-the-counter medications that also can cause problems. For example, your doctor can review your heart medications and avoid prescribing medications that when mixed with Aspirin and supplements such as omega-3 fish oil and garlic are known to cause problems with thinking ability. Healthcare practitioners are instructed to consider the following issues in a handbook from the U.S. Agency for Healthcare Research and Quality:
- Whether drugs you are taking are incompatible (medication reconciliation).
- Where you obtain your drugs (medical procurement).
- Whether you are not taking the medications and the reasons why (intentional nonadherence).
- Keeping track of how you are doing while taking your medications (ongoing monitoring).
Medicines are part of the reason that modern healthcare has had a tremendous impact on death and disability. However, remember that all medicines can have side effects, especially when taken together.


The comments section is closed.
Please also speak to your pharmacist! We are the medication experts and are especially knowledgeable about drug interactions. We are actually trained in deprescribing and can help with tapering a meducation to a lower dose or discontinue it.
Over 40% of trauma patients 45 years and older were receiving 5 or more medications at the time of their injury (1). There are many definitions on polypharmacy exist in the literature, but as emphasized by the Lotfipour and Vaca (2) there is little disagreement about the effects medications can have on the daily functional aspects of our senior citizens. As Lococo and Staplin (3) noted that the physicians who routinely care for them may not be giving enough consideration to the cognitive and motor impairment attributable to polypharmacy’s placing older adults at increased collision risk (2, 3). Polypharmacy effects on falls, activities of daily living, cognitive agility, and driving fitness, coupled with older adult physiologic changes, can have a significant impact on our health care system. AGS Beers Criteria® includes lists of certain medications worth discussing with vulnerable elderly older drivers because they may not be the safest or most appropriate options for these injury prone high risk driver populations.
References:
(1). Evans DC, Gerlach AT, Christy JM, et al. Pre-injury polypharmacy as a predictor of outcomes in trauma patients. Int J Crit Illn Inj Sci. 2011;1(2):104-109. doi:10.4103/2229-5151.84793
(2). Lotfipour S, Vaca F. Commentary: Polypharmacy and older drivers: beyond the doors of the emergency department (ED) for patient safety. Ann Emerg Med. 2007;49(4):535-7.
(3). Lococo K. and Staplin L. Literature Review of Polypharmacy and Older Drivers: Identifying Strategies to Study Drug Usage and Driving Functioning Among Older Drivers, National Highway Traffic Safety
Association (NHTSA, 2006) Publication No. DOT HS 810558.