Lack of access to primary care is a constant theme in health-care discussions. Family physicians and nurse practitioners are overwhelmed by the sheer magnitude of the tasks they face, and many are retiring from practice. Various strategies are being proposed to address these problems – problems that will certainly require multiple solutions.
One strategy increasingly being recognized is direct access to interprofessional members of primary care teams. Timely, direct access to physiotherapy, for instance, has demonstrated significant reductions in pain and improved function for patients while reducing the number of primary care physician appointments related to pain. A study published in 2010 showed that in one year, almost one out of four Ontarians (22.3 per cent) saw a physician about a musculoskeletal (MSK) problem; 83.2 per cent of these visits were to primary care physicians. These problems included arthritis, acute injuries and chronic pain, all of which can be assessed and managed by physiotherapists.
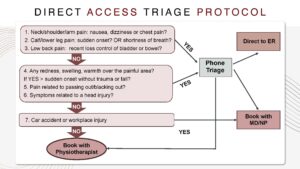
Through the use of a simple scheduling algorithm, many MSK clients in multidisciplinary primary care settings can be booked directly with a physiotherapist, thus safely bypassing initial appointments with a family physician or nurse practitioner. This approach has been effectively employed by multiple community health centres in Toronto since 2016.
Currently, only 40 out of 297 primary care teams (including family health teams, community health centres, nurse practitioner-led health clinics and Aboriginal health access centres) in Ontario have physiotherapists. Since 25 per cent of Ontario’s population receives primary care through these teams, and as the province looks to invest $30 million to establish 18 new interprofessional primary teams, expanding funding to include physiotherapy in all team-based care models would be an easy win for the system.
Access to physiotherapy in these teams could also be made available to patients attached to local solo practitioners, and to those who do not have a doctor or nurse practitioner at all (2.2 million Ontarians as of March 2022, according to research data). This type of partnership has already been successfully implemented in West Toronto. Expanding the role of physiotherapists to include ordering diagnostic imaging and initiating specialist referrals would further ease the workload of family physicians and make more effective use of scarce human health resources.
The United Kingdom already has implemented this model on a national scale. Starting in 2018, physiotherapists were deployed in clinics across the U.K. as Musculoskeletal First Contact Practitioners. An audit of the program showed that 98.3 per cent of patients did not need follow-ups with their general practitioners, and there was a high level (97.4 per cent) of patient satisfaction. The audit did note that sufficiently increased numbers of physiotherapists and successful marketing of the program is required to make a sizable dent in the enormous burden of care that musculoskeletal problems bring to the system. As with everything else, effectiveness requires commitment.
Booking directly with a physiotherapist for a musculoskeletal problem is nothing new. People who can afford it, or have benefit plans that cover physiotherapy, already can book their own physio assessments at private clinics. However, many Ontario residents cannot afford private physiotherapy, meaning they seek care from their family physician or nurse practitioner for conditions that a physiotherapist could, and should, effectively manage. Physiotherapists have the training, knowledge and skills to perform initial assessments and develop effective treatment plans for acute and chronic musculoskeletal problems; they also have the skills to recognize when a condition does require medical attention (for example, a possible fracture).
Some may fear that employing physiotherapists requires a large investment in gym-sized spaces and exercise or treatment equipment. However, this is not the case. Physiotherapy assessments and highly effective exercise programs can be performed in regularly equipped clinical offices.
As one of the authors of this article and a family physician, I can personally attest that patients have an improved quality of life when working with physiotherapists, and staff at community health centres have a deep satisfaction for the overall improvement in care that is provided.
Increased access to the right care by the right provider at the right time benefits everyone.


This is such an important topic! But one, while touted for by many in the rehab sciences’ field, particularly physiotherapy (PT), in N America, not shown to be of direct value in primary care (PC) prior to the post by Emily and Wendell. What is so relevant is that it has been easy to set up, well accepted by other primary care providers (PCP) team member’s, and active in a number of different team based care settings in the W Toronto area, and, ongoing for some years! The concern about ordering diagnostic imaging and making referrals creating an added burden is only real if the PTs are not empowered to do this directly. Terrific cutting edge innovative Stuff!
“Expanding the role of physiotherapists to include ordering diagnostic imaging and initiating specialist referrals would further ease the workload of family physicians and make more effective use of scarce human health resources.”
You had me until this. This is the trope that has been utilized by other health care professionals to expand their scope of practice and I am disappointed to see ‘easing the workload of family physicians’ as rationale to expand the role. If it creates another silo where additional paperwork/administrative burden is dumped on a family physician’s desk…like has happened with other scope expansions…it further kills community based family practice. Fine…work within a team…that would be good for easing the workload. But allowing any physiotherapist in any strip mall to order imaging and refer to specialists is going to fragment care further