Reaching adulthood should be a celebratory milestone, filled with greater independence and possibilities for the future. But for the estimated 200,000 young Canadians with disabilities, turning 18 often feels like falling off a cliff.
Instead of empowerment, they face a fragmented, siloed adult-health care system – a sharp contrast to the “one-stop shop” model of the pediatric system. A critical piece of this transition is missing: timely, coordinated access to interprofessional teams of specialists with essential expertise in disabilities and neurodevelopmental differences. As a result, the shift to adulthood becomes even more daunting.
Once they transition out of pediatric care, young adults must navigate a complicated landscape marked by waitlists, knowledge gaps and a lack of resources. In Canada, research suggests that around 70,000 medical transitions for youths with disabilities and chronic illnesses occur every year as they turn 18. Unfortunately, system shortcomings often result in more emergency department visits, hospitalizations and significant health setbacks.
“The adult health-care system is like a shopping mall, except the shopping mall has one store that’s open at weird times and is five hours away from your house. Now, I have to go to five different places for everything that I need. The fact that my care is not in a centralized place makes it difficult to arrange scheduling and keep track of everything.” – Rachel, 21
Consider the case of a young person with spina bifida. After leaving pediatric care at 18, they relied on home care for regular catheter changes but never saw an adult urologist. A decade later, they arrived at the emergency department with sepsis – a life-threatening infection – and severe ulcers. Such preventable issues underscore the urgent need for better transitional care to improve long-term health outcomes.
In 2024, Holland Bloorview Kids Rehabilitation Hospital, a leader and a catalyst for system solutions to support better health care for children with disabilities, brought together a team of clinicians, young adults and caregivers to design a survey to understand the experiences of young people with disabilities. The results have been collated into a first-of-its-kind report that underscores the serious medical challenges faced during this transition. Two-thirds of young adults with disabilities report unmet health-care needs; half continue to rely on pediatric providers due to a lack of adult care. Moreover, over a third of these young adults either wait more than three years for a family doctor or still haven’t found one at all.
Joseph, 17, who has cerebral palsy and uses a power wheelchair. He expresses the anxiety many face: “I’m scared about what will happen when I need support [when I turn 18].”
Fortunately, solutions are already afoot. With initial investment and strategic, forward-thinking approaches, health-care teams from pediatric and adult systems are creating collaborative transition clinics. These clinics are designed to ensure young people can seamlessly access the care they need as they transition into adulthood.
This model has shown promise at Holland Bloorview, Sunnybrook and The Hospital for Sick Children, where we are piloting a virtual urology transition clinic for youth with spina bifida and spinal cord injuries. The clinic provides more equitable, accessible and interprofessional support that helps to maintain continuity of care as patients move into adulthood.
Holland Bloorview, alongside its adult health system partners, is continuing to move the needle by understanding the issue, convening the experts and conducting research to create the urgent change necessary to improve access and streamline the transition from pediatric to adult health care. This research, as well as training and resources, are prerequisites to this needed evolution. This, of course, can’t happen without dedicated funding from government and philanthropic sources.
In an ideal world, we won’t call it pediatric and adult care anymore. We’ll just think of it as life-long care, where everyone – including young people with disabilities – receives the right services at the right time to support their health and well-being.
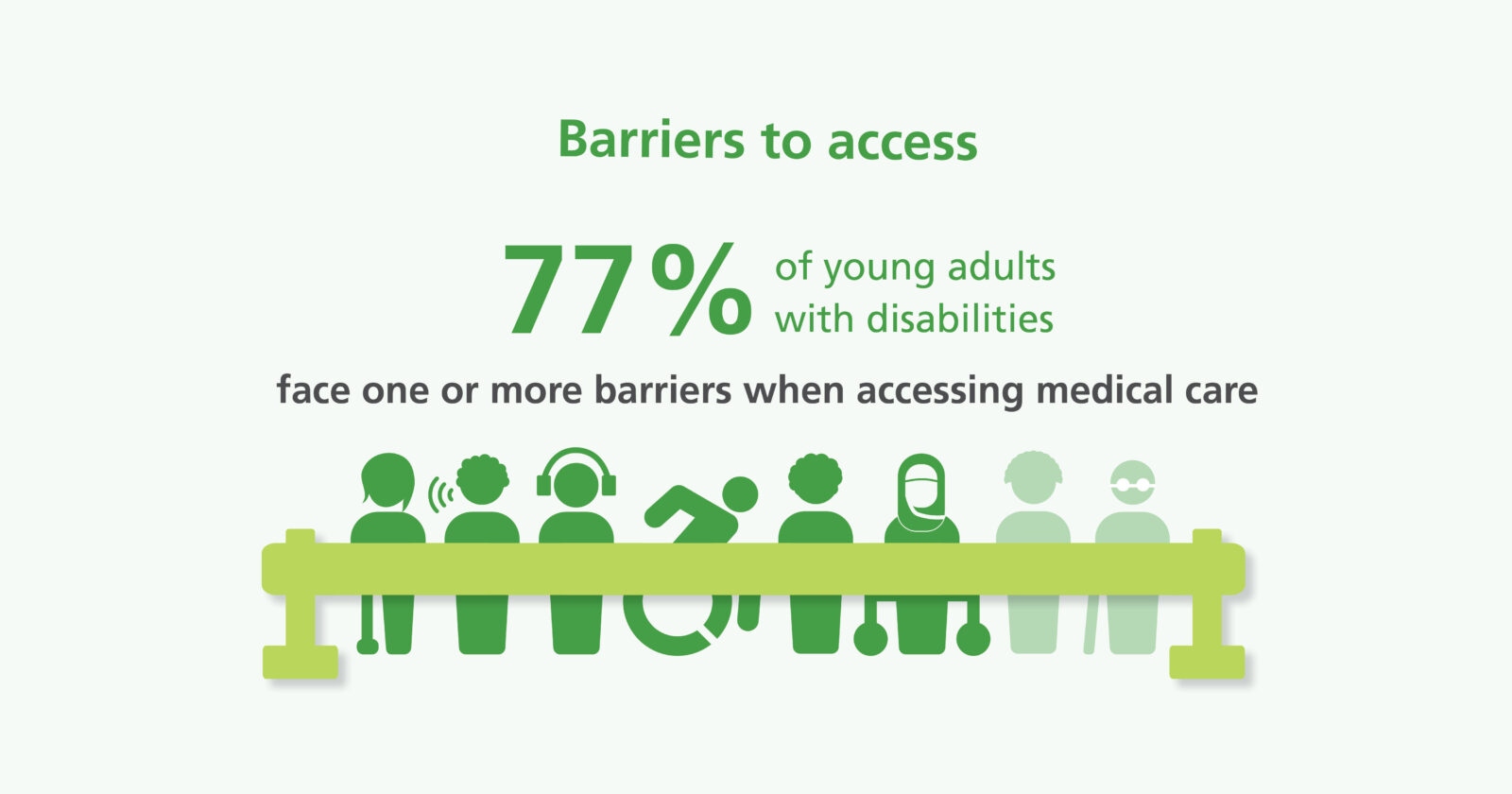
- 49% experience attitudinal barriers such as feeling judged, ignored or treated as inferior by health-care providers. This highlights how ableism may be preventing young adults from getting the care they need.
- 32% experience informational barriers, meaning they have received medical information in formats that did not suit their learning, vision and/or hearing needs. This sheds light on the fact that many young adults with disabilities may be struggling to receive medical information in formats that work for them, making it hard to ask questions or understand their health-care needs and treatment plans.
- 23% experienced physical barriers when going to medical appointments such as narrow doors and hallways, inaccessible washrooms that cannot accommodate large wheelchairs, and lack transfer lifts to lay on exam tables or in exam chairs.
- 14% experienced barriers related to transportation such as finding accessible vehicles – like cars, vans or buses with ramps – for medical appointments.
- 11% faced technological barriers such as lack of access to screen software or closed captioning. These barriers may impact an individual’s ability to engage in health-care discussions and access crucial health information, leading to frustration and disconnecting from the health-care system.



The comments section is closed.
Thank you for writing and publishing this article. It addresses a very important issue in care for people with disabilities. Transitioning into adult care programs can also have significant problems in terms finding adequate and appropriate housing. Thank you.
Thank you for your feedback. Your support is important in advocating for an integrated system and better transition care owed to every young adult with chronic condition and/or disability transitioning from paediatric to adult healthcare system.