Grace (name and some details changed to protect her identity) is a nine year old girl who lives in the northern suburbs of Toronto. Her doctor diagnosed her with asthma last year, and developed a care plan and prescribed her medication. Grace’s family understands and agrees with the care plan. But Grace’s acute attacks have continued, and she has been to the Sick Kids’ Emergency Department repeatedly over the past few months.
At first her doctor assumed that Grace’s family was not following the care plan, but after her most recent trip to the Emergency Department, Grace’s doctor learned that the family’s home has a mold infestation – a known trigger for asthma – but the landlord has refused to have the mold removed.
There is a growing movement within health care to treat – or even prevent – health problems like Grace’s with social, rather than medical, interventions.
While social services such as legal aid already exist outside of the health care system, a growing number of Canadian health care organizations are experimenting with adding professionals such as lawyers and financial experts to health care teams. By embedding these non-health professions as members of health care teams, these organizations hope to improve access to these social services and ultimately, to improve the health of their patients.
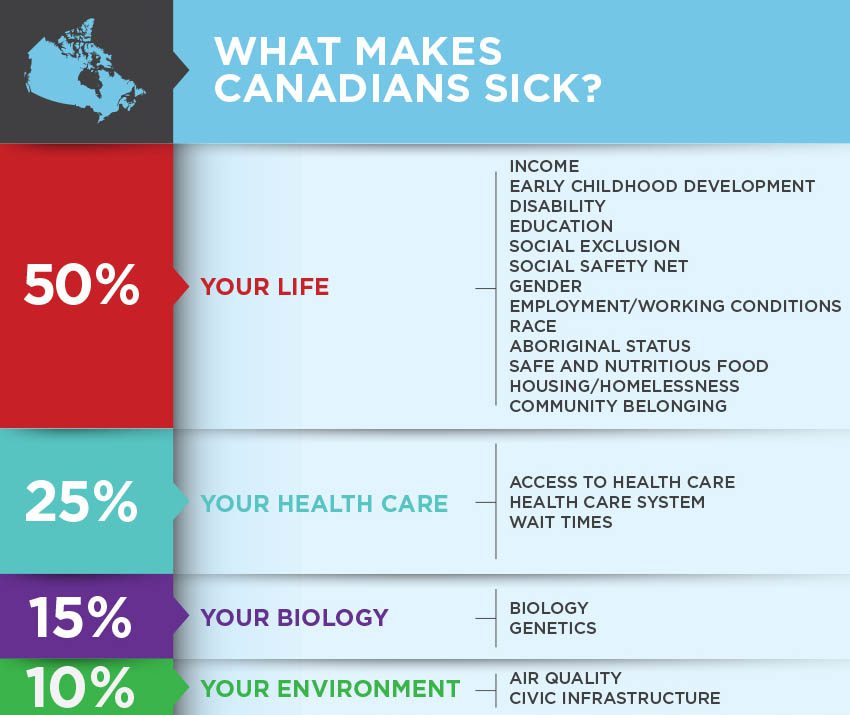
Social determinants of health
At a population level, social conditions such as employment, income, housing, education, and access to nutritious food have a larger impact on health than someone’s genetics, lifestyle choices or access to health care services.
While these social conditions extend well beyond the walls of hospitals and doctors’ offices, the health care system has made some efforts to address them. Chief among these has been the relatively long standing efforts to increase the role social workers play in both acute and primary care settings. Social workers can help patients address social issues such as housing and income. Efforts to introduce lawyers and financial experts into health care teams build upon this model and expand the range of social determinants that can be addressed from within the health care system.
Medical-legal partnerships
Formal partnerships between lawyers and health professionals began in the United States more than 20 years ago, and now include 262 health care organizations in 36 states.
“Legal problems are health problems,” explains Kate Marple of the National Centre for Medical Legal Partnership at George Washington University. According to Marple’s organization, many of the social conditions that negatively affect health can be traced to laws that are “unfairly applied or under-enforced,” and so many of them have a legal remedy.
At Canada’s first medical-legal partnership – between Sick Kids and Pro Bono Law Ontario (a charity established to respond to unmet legal needs) – four-hundred patients a year access an in-hospital lawyer to receive help with legal issues that include immigrant/refugee law, family law, education law, employment law, and health law.
At Sick Kids, medical staff and social workers can refer patients to a “triage lawyer”, who works in the hospital. The triage lawyer can deal with many issues on site, or can refer patients with issues requiring specialized legal services to one of Pro Bono Law Ontario’s partnered law firms. In addition to providing specific legal services, the triage lawyer also provides education to patients about their legal rights and to health care professionals about how to recognize legal problems.
One of the early successes of medical-legal partnerships was to identify patients like Grace whose asthma attacks were being triggered by poor housing conditions such as mold, cockroach or rodent infestations. By taking legal action against delinquent landlords, in-hospital lawyers were able to improve the patients’ housing conditions, which reduced their asthma attacks, explains Lynn Burns, Executive Director of Pro Bono Law Ontario.
This type of intervention was found in a small US-based study to be associated with a substantial decrease in asthma patients’ Emergency Department use and hospital admissions, as well as a reduction in medication use. In addition, both a literature review of medical-legal partnerships and an evaluation of the Sick Kids partnership have documented meaningful benefits to patients and their families, such as decreased stress related to the child’s health and improved financial condition. While medical legal partnerships have yet to be studied with a randomized control trial, evidence to date suggests that some health problems may be more effectively treated with legal remedies than with medical ones.
According to Burns, there is significant demand for these partnerships. Since establishing its first partnership five years ago, Pro Bono Law Ontario has created three more with Children’s Hospital at London’s Health Sciences Centre, the Children’s Hospital of Eastern Ontario in Ottawa and Holland Bloorview Kids Rehabilitation Hospital in Toronto, and another beginning this October with McMaster Children’s Hospital in Hamilton.
The demand may be even greater in primary care. In preparation for launching Canada’s first primary care-based medical-legal partnership, St. Michael’s Hospital and ARCH Disability Law Centre conducted a needs assessment for the hospital’s Family Health Team, which serves about 34,000 patients in downtown Toronto. They found that more than half the patients referred to their social workers – 1,980 patients – had at least one legal issue, and many had two to three, according to Nav Persaud, the physician spearheading the initiative at St. Michael’s.
Financial expertise in primary care
While some patients’ health problems can be addressed through the law, others suffer from health problems caused by having too little income to afford adequate food or housing. To help these patients, some doctors are experimenting with embedding a financial expert into their care team.
Family doctors at the St. Michael’s Family Health Team can now write a prescription for income security, much like they prescribe medications. Patients who receive this prescription see the in-house income security health promoter, Karen Tomlinson.
St. Michael’s Hospital’s income security health promoter referral form
Tomlinson helps patients raise their incomes through a number of avenues, from applying for government subsidies to conducting tax clinics. She also works with them to reduce their expenses by helping them access discounted or free services. Another important function of the role is to improve patients’ financial literacy, which can help stretch limited budgets, as well as avoid fraud and predatory lenders.
While this approach is new to Canada, the United Kingdom has had a similar system in place for a number of years. UK studies that evaluated this approach have found that roughly one quarter of patients who used the service benefited from it financially, on the order of £100-200 per month ($180 to $360 Canadian dollars). However, a small randomized control trial looking at patients over 60 years of age was unable to detect any improvements in health status associated with this program, though qualitative interviews with study participants suggested that the program helped them navigate the system, allowed them to buy more nutritious food, and improved their quality of life. A larger randomized control trial of the UK program is currently underway.
The St. Michael’s program is also being evaluated with a randomized control trial. “While the evidence that social factors influence health is very well established at this point, we don’t yet have the same quality of evidence about which social interventions are most effective at improving health,” says Andrew Pinto, the study’s principal investigator and a doctor in the Department of Family and Community Medicine at St. Michael’s. The trial will measure change in income, expense reduction and change in finance literacy.
While the results of the trial will not be available for a few years, the program is proving extremely popular. “My patients love it – it’s made a big difference for several of them,” says a family doctor not associated with the study.
“Breaking down silos”
Providing legal and financial services to low income individuals is not in itself new. But these programs differ from traditional service models by co-locating legal and financial experts within health care teams.
Embedding legal and financial professionals within health care teams brings a number of important benefits, according to Pinto. “People with legal or financial trouble often feel a great deal of stigma,” he explains, “and so many of them are reluctant to seek out the services they need. But when a doctor says to them ‘this problem you have – this legal or financial problem – this is a health problem.’ That can be very powerful in reducing the stigma,” he says.
Ivana Pericone, Executive Director of ARCH Disability Law Centre, explains that another key benefit of this model is accessibility. Some people either do not realize they have problems that legal aid can help with, or do not know where to find this help. By locating legal aid services alongside the health service many of them are already using, and training medical providers to spot legal problems that may be contributing to ill health, lawyers can better reach the people who need their services.
Marple believes one of the greatest benefits is that these models are “breaking down silos,” and allowing for a truly comprehensive approach to treating health problems that have both social and biological roots. Persaud agrees, saying “we can do more together.”
Sustainability and scalability
One of the chief challenges faced by innovative programs like these is finding stable funding.
Unlike medical services that are paid for through the Ontario Health Insurance Plan, legal and financial programs within health care are currently funded by a range of charitable and non-profit organizations.
For example, the partnership between Sick Kids and Pro Bono Law Ontario is supported through core funding that Pro Bono receives from the Law Foundation Society of Ontario and the Law Foundation of Ontario, which are both charities. This can create significant challenges when it comes to scaling up-programs like these, as charities likely do not have the capacity to meet provincial – let alone national – demand.
This is a barrier not just for these programs, but for virtually all interventions aimed at social determinants. The incorporation of legal and financial professionals in care teams is certainly part of what the World Health Organization (WHO) Commission on Social Determinants of Health had in mind when it recommended “acting more coherently through the health-care system to target social causes of poor health.” But even when these programs prove cost-effective, the siloed nature of governments means that the “coherent, cross-sectoral financing” recommended by the WHO commission is rarely achieved in practice.


The comments section is closed.
On this pandemic, no one has an idea why I’m so happy and living large in a bit. It is Engr. Rodriguez Blank Credit Card, is the best financial help. I came across him on YouTube Josephine was talked about how she became rich with Blank credit card, immediately I contacted him and purchase for the Credit Card of $30,000 for 1 year and 6 months last week and I receive my card on Monday through Fedex courier immediately I ran down to close by shopping more with my pin to shop some shoes and clothes it work like a magic it was unbelievable, I thought I’m going to get caught I was surprised my stuff was given to me, This time I fully recommend him to anyone who need his credit card he is real and trustworthy. Contact him now and get yours and live large. I’m a living person. This is not fake, it is real.Our government does not care about us. Email:rodriguezatm@outlook.com. Thank you Rodriguez, God bless you.
This is an inspiring endeavor. Congratulations, and thanks for helping clarify my thinking about the interface between medical and legal problems.
Community Health Centres in Toronto and Ontario have been doing such type of work for many years. Ensuring individual patients and families access legal aid, immigration consultants and lawyers, nutritionists, housing workers, educational and workplace opportunities, ensuring that people on social assistance receive the few benefits they are entitled.
We need to ensure via political advocacy that the model of Community Health Centres remains loud and strong in the current provincial agenda.
Great to hear about research being done re such impact within this specific model.
thank you
anne egger
Addressing the social determinants of health and integrating services is essential to improve health. I worry about the model where once again the physician is the gate-keeper. Another prescription for income security or legal advice. More money for healthcare so we can add professionals to the healthcare team. Why is healthcare at the centre of this, why isn’t it social services or education? There is no end to what can be subsumed in the name of medicine and healthcare. I think this is more like a horse and carriage situation then a chicken and egg. Let’s tackle the really big issues, such as poverty, inadequate housing, education or just any one of them as creatively as we seem to trying to solve health issues and then, as all the literature suggest, health of both individuals and the population at large will improve.
It’s not Just the Legal and Financial problems themselves that have an adverse effect on a person’s health status; the Stress associated with having to cope with major Legal or Financial problem can also have a significant impact on someones physical and mental health and well being. Stress has been clinically proven to be a factor in the increased incidence of Hypertension, Heart Attacks, and Nervous Breakdowns among other health problems. Stress may also cause some people to overindulge in food or alcohol in an attempt to make themselves “Feel Better”. And that can cause an increase in the rates of Obesity and Alcoholism; which can in turn, cause other health problems. Financial problems have also been known to cause Relationship Problems which can cause the break-up of Marriages and Families; and deprive someone of one of their Basic Essential Support Systems – (The Family Unit) – at a time when they may need it the most. And that can have a significant impact on how a person copes with Medical, Legal, and Financial problems; making the situation worse. Helping someone with their Legal and Financial problems while their receiving treatment for their Medical problems could significantly reduce their stress levels and enable them to concentrate more fully on improving their Mental & Physical Health and Well Being. And that could Dramatically improve their chances of having a positive outcome. I think that it’s an excellent idea to integrate Legal and Financial Services with the Health Care System; because their are many people in our society who may not be aware of their Legal or Human Rights in this country, Such as new immigrants and those who are functionally illiterate. And there are others who may be aware of their rights but lack either the knowledge or ability to successfully advocate for themselves. And there may also be some individuals who may realize that they need Legal or Financial Help; but lack either the knowledge or resources necessary to obtain the help that they need. Just as the CCAC helps people to access the right Medical Services & Professionals at the right time; an Integrated Medical, Legal, and Financial Services System could also help people to have access to Justice & Financial Assistance in a Timely manner. That in turn could lead to an improved quality of life which could improve the overall Health and Well Being of our Society. And with fewer people getting sick, there would be a lot less of a strain on our Health Care System. And the improved Health of our community could also lead to increased productivity as a result of fewer people calling in sick. And that in turn would give our Economy a boost.
I work as a primary care provider in a community health centre (CHC), providing services to an inner city population. We know exactly how important it is to include all disciplines in a multidisciplinary approach, including legal and financial “care” providers. I am pleased to have this issue brought up for discussion, as it increases our awareness of how central these issues are.
Effective CHCs like ours–which exist across Canada and the US–have been doing this type of silo-busting on a less-structured, case-by-case basis for years. We have found the best benefit comes from a “gradual creep” toward better understanding amongst disciplines, building of relationships and cooperation amongst providers, and better outcomes.
I will be watching with interest the results of the randomised controlled trials (really?) on this intervention. I’m looking forward to being convinced that “in-house” services are superior to a robust, well-connected and locally-situated multidisciplinary system of service connections. I suspect that is not an arm in the trial.
The real question for me is: is there a place or person that people with legal problems can go to, where they’ll receive a “prescription for health security” which gets them connected with primary care or other appropriate healthcare needs?
Until we as healthcare providers break down our own hieracrchical silos, and move away from unjustified assumptions about how care should be provided, I think there’s a bit of hubris in talking about how hard we work to break down these other silos.
This is brilliant! There is potential here for Alberta’s Primary Care Networks (if funded more robustly, particularly the smaller ones) to make a much bigger difference in patient’s lives than they’re already making.