I want a primary-care provider with whom I can build a long-term relationship and who understands my health-care needs.
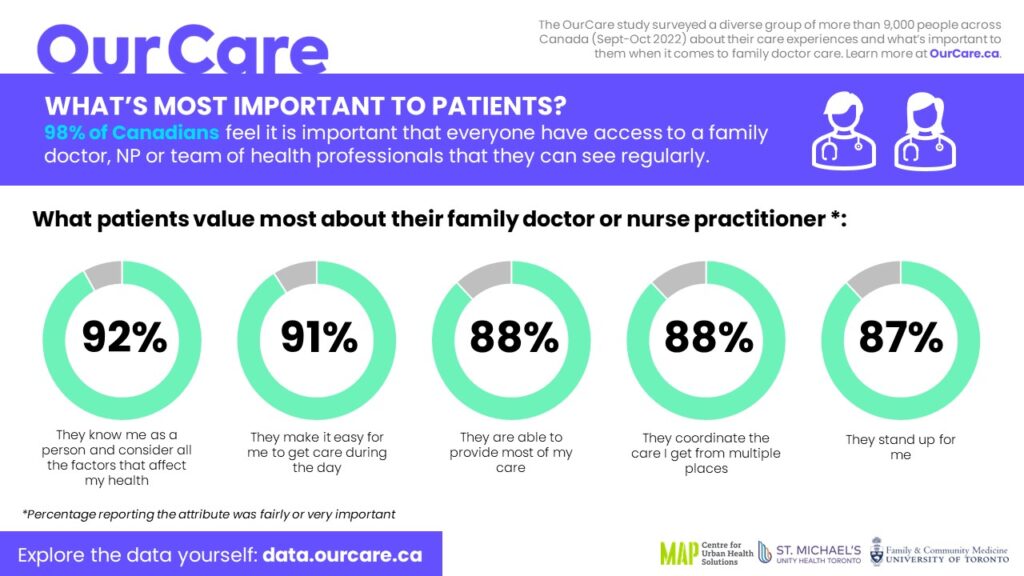
That’s the message that comes through loud and clear from an online survey of more than 9,000 Canadian adults last September/October as part of the OurCare initiative to engage the public on the future of primary care.
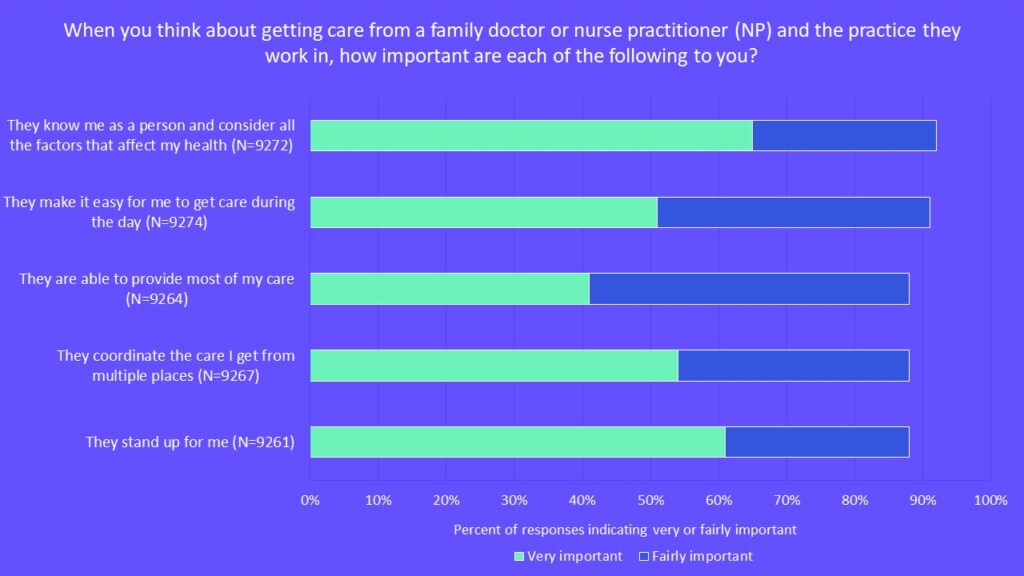
People were asked to think about their past experiences with the health-care system and what they value. They were then presented with 10 dimensions of primary care and asked the importance of each one to them. Response options were based on a validated set of questions used to measure quality in primary care from a patient perspective.
The results made it clear that what people consider most important is that their primary-care provider “knows me as a person and considers all the factors that affect my health.” The top five responses chosen as either fairly or very important, in order, were:
- They know me as a person and consider all the factors that affect my health.
- They make it easy for me to get care during the day.
- They are able to provide most of my care.
- They coordinate the care I get from multiple places.
- They stand up for me.
Having a primary-care provider who knew them was particularly important for women and those of diverse gender; seniors over age 65; people at the lowest income level; those reporting poor health; and those reporting having a disability.
Our results highlight that an ongoing relationship between a clinician and patient is central in primary care.
As a patient/caregiver advocate and family physician, respectively, we’ve seen the benefits of relationship-based care first-hand. Relationships build trust, allowing patients to feel comfortable revealing aspects of their lives they may have kept hidden due to shame and fear. Relationships build a mutual understanding of underlying values that drive care decisions. Relationships enable effective listening and dialogue to understand a patient’s story and consider a physician’s advice. Relationships help clinicians know a patient’s health history but also see the whole person in the context of their families and community and the journeys of their lives.
Dozens of studies have confirmed the value of a continuous relationship. When patients see the same family doctor for most of their visits instead of a different family doctor for each visit, both patients and the system benefit. Studies have shown that patients are more likely to get recommended preventive care, follow through on treatment recommendations, have better health outcomes – and even that they are less likely to die. Studies have also shown higher care continuity relieves stress on the health-care system as a whole, including fewer emergency department visits and overall cost savings.
The OurCare survey results add to the research evidence, reinforcing that care continuity is an important priority for patients and the public.
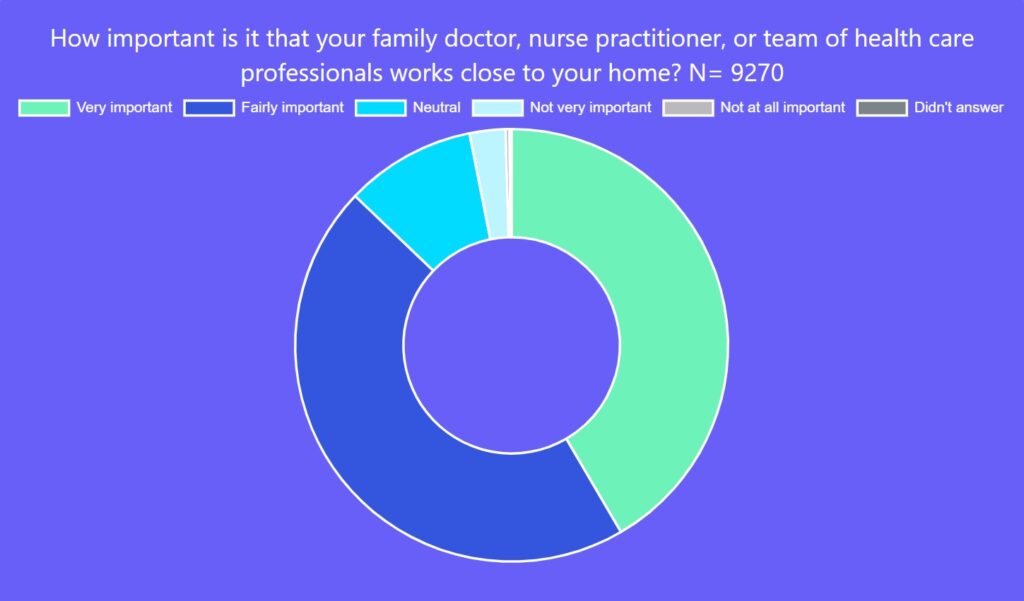
Getting primary care close to home was also a top priority. An overwhelming majority of those responding said it was very important (42 per cent) or fairly important (46 per cent) that their family doctor, NP or team of health-care professionals work close to the respondent’s home.
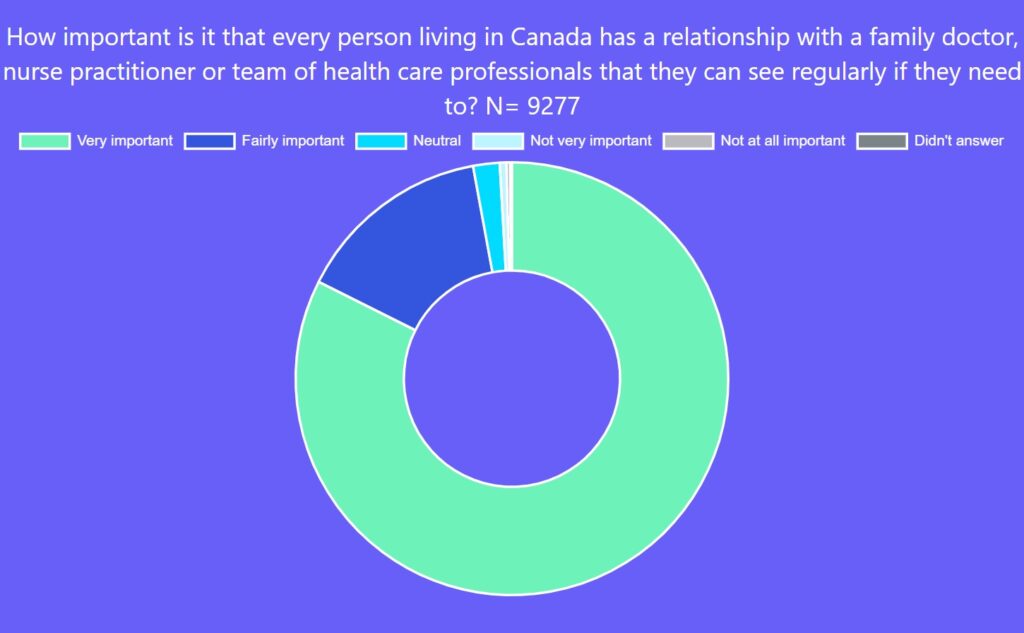
Ninety-eight per cent of respondents said it was very or fairly important that every person in Canada have a relationship with a family doctor, nurse practitioner or team of health-care professionals they can see regularly when needed. Unfortunately, too many people in Canada struggle with having any access to primary care, a situation that has worsened over the course of the pandemic.
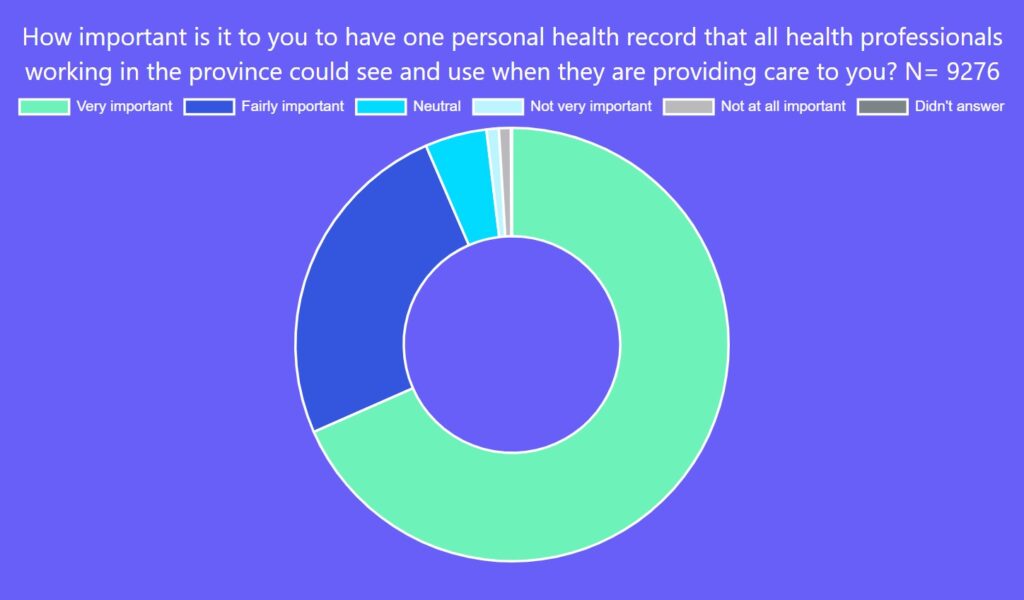
In addition, 75 per cent of Canadians said it is important to have online access to their health information and 93 per cent noted it is important to have one personal health record that all professionals caring for them in the province can use. This, though, is far from reality for most.
Some provincial governments have implemented short-term solutions to address the crisis, increasing the number of urgent care centres or virtual walk-in clinic options. But ultimately, these are band-aid approaches that don’t align with the kind of care people really want.
The findings of the OurCare survey reinforce principles that have long been valued by many in the primary-care community: relationships matter; continuity matters; understanding patients as whole people matters.
People want timely care, close to home, delivered by a primary-care clinician who knows them, stands up for them, coordinates their care and helps them meet their health goals. Let’s design care around those priorities.
Explore the data yourself at data.ourcare.ca. For more information about OurCare, visit OurCare.ca.


The comments section is closed.