The number of Canadian medical graduates unmatched with a residency training program has reached unprecedented levels, with students and faculty concerned about the growing gap between students and necessary training.
Since 2009, the number of unmatched Canadian graduates has been steadily increasing, moving from 11 in 2009 to 68 this year.
“This represents 68 students who have spent on average eight to 10 years of undergraduate education to become physicians, incurring great debt, and utilizing taxpayer dollars to facilitate their education,” says Mel Lewis, a student affairs associate dean at the University of Alberta.
“There’s a lot of anxiety,” says Franco Rizzuti, president of the Canadian Federation of Medical Students. “Students are starting to grasp at straws, trying to understand what’s going on.”
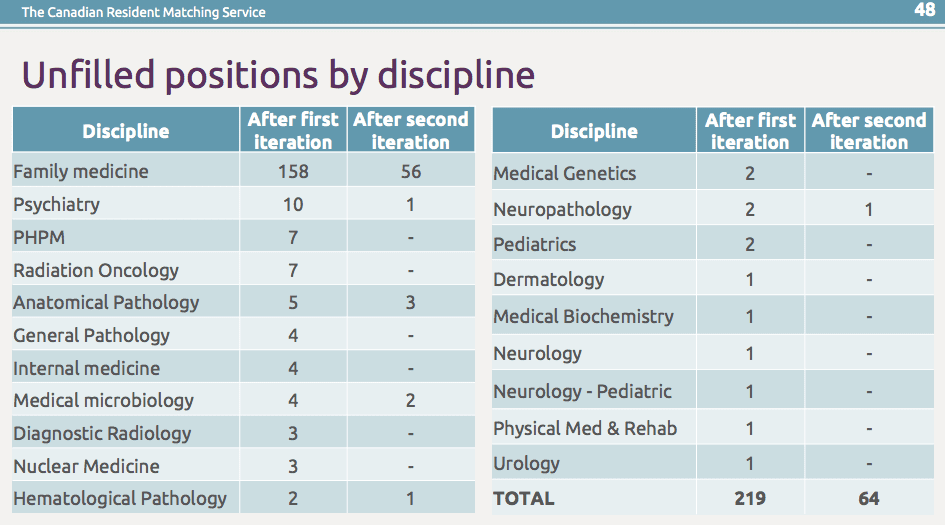
A total of 64 training positions also went unmatched, including four in Alberta, two in Ontario and 58 in Quebec.
To be able to practice medicine, all medical students need to complete a residency program in an area of specific clinical medicine, such as family medicine, surgery or psychiatry. Students compete with each other for a residency program through an application and matching process administered by the Canadian Resident Matching Service (CaRMS). This follows a very similar process to the one used in the United States.
From a broader societal perspective, those who track health human resources nationally say there’s no reason to panic: 68 unmatched participants is a small fraction of the nearly 3,000 Canadian medical students who took part in this year’s match, and the 64 positions that remained unmatched typically end up filled.
On an individual level, although being unmatched is stressful and a loss of a year, historically, virtually all unmatched students find success in subsequent years.
Matching for a physician’s future
In many ways, the Canadian medical residency match isn’t all that different from online dating: following a written application and interviews, students and training programs rank one another and an online algorithm is used to identify potential matches. In essence, both parties need to “swipe right” to make a match.
However some training programs have fewer positions than applicants and other programs don’t have sufficient applicants of interest for their positions.
There are two iterations of the match; the first is reserved for newly-graduated Canadian medical students. Students unmatched in the first round, as well as international medical graduates (including Canadian citizens studying in medical schools abroad) and Canadian medical graduates who went unmatched in previous years, join the second iteration.
A student may choose to apply to only one program – training in cardiology at McGill or paediatrics at the University of British Columbia, for example – or rank multiple programs in multiple locations.
Rizzuti says students apply to an average of 18 programs – nearly double the number of program applications compared to a decade ago. CaRMS data show there were 128,334 applications to 644 programs, up nearly five percent over last year.
Historically, the match has had more wiggle room in the first round and a greater likelihood that Canadian medical graduates would match with their top-ranked training program.
In 2009, the ratio of Canadian medical graduates versus residency positions was 1:1.12.
“There was a little bit of a buffer in the system, a few more spots than there were Canadians applying. That gave some flexibility and allowed international medical graduates to come into the system,” says Genevieve Moineau, president & CEO of the Association of Faculties of Medicine of Canada.
In 2017, the ratio shrank to 1:1.026. “Now instead of having a 10 percent buffer, you’ve got a 2.6 percent buffer. It’s really, really, really tight,” Moineau says.
Mismatch in student interests versus training needs
The number and types of training positions available are usually decided by governments and medical schools, based on planning for population needs and medical school capacity. The exact process varies by jurisdiction, with population needs beginning to drive the process in some provinces.
The overall number of residency positions available across Canada has remained largely unchanged since 2013, when it rose above 2,900. (Last year, the quota was 2,970. This year it was 2,967.)
But the number of graduates participating in the match has outpaced growth in the quota. In 2013, there were 2,633 Canadian medical graduates participating. This year, that number rose to 2,810, a slight dip from 2016, when 2,836 medical graduates were looking for a match.
“There has been a decline in residency spots, most notably in Ontario, with no commensurate decrease in medical student enrolment, squeezing the supply and demand quotient even further,” Lewis says.
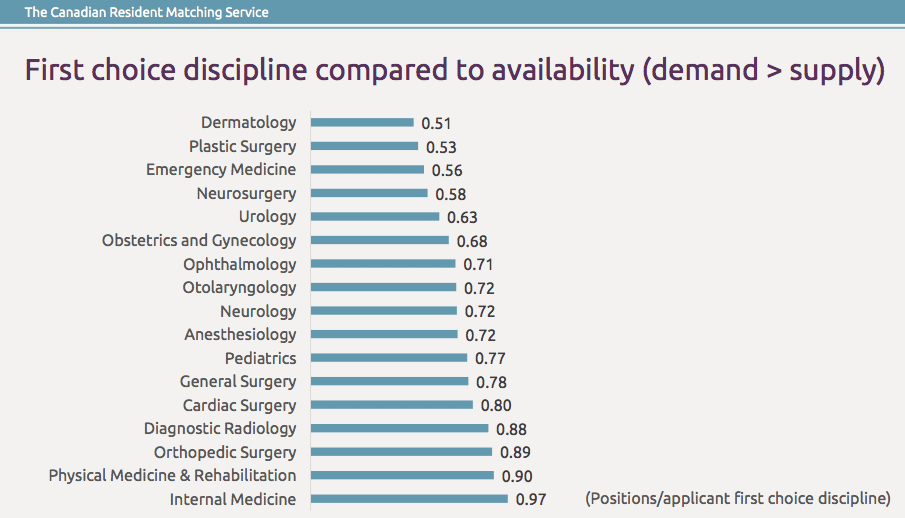
Exacerbating this tightened ratio is a long-standing mismatch between the personal career interests of medical students and where governments have funded training positions based on their view of future physician need.
Some say it is an unreasonable expectation that every medical graduate should have the residency of their choice.
“It’s, in part, the mindset,” says Ivy Lynn Bourgeault, who holds the Canadian Institutes of Health Research Chair in Gender, Work and Health Human Resources and is lead coordinator of the pan-Canadian Health Human Resources Network. “We should go where the need is. That should be inculcated in medical schools.”
This year, graduates ranked dermatology, plastic surgery and emergency medicine highest, with demand for training in those disciplines far outstripping the supply of training spots.
By contrast, after the first and second rounds of the match, opportunities in family medicine, psychiatry and laboratory sciences (which includes different types of pathology) were left unfilled.
This year’s match also saw a slight reduction in the number of students prioritizing family medicine and more students ranking internal medicine, creating a wrinkle for students who could not have anticipated this shift and failed to give themselves options in their rankings.
Applications from international medical graduates (IMGs) may also be a factor, putting more pressure on Canadian students looking to match in the second iteration. The number of IMGs participating in the match peaked at more than 3,100 in 2014, when the Objective Structured Clinical Examination became a mandatory requirement for all IMG applications outside of Saskatchewan. This year more than 2,400 IMGs participated.
But Bourgeault argues that IMGs are not the problem, citing forthcoming research. “We under-utilize immigrants,” she says, noting that many of the IMGs who find success in the match process are willing to go where others won’t.
Migration out of Quebec
Migration within the country is also playing a role, with students in Quebec opting for residencies in other parts of the country. While bilingual students can rank positions in Anglophone Canada, English-speaking students can’t hope to place with a training position that requires French.
This year’s match shows that while Quebec had 58 unfilled positions, it had only eight unmatched graduates, compared to 35 unmatched graduates from Ontario, 20 from Alberta and five from Atlantic Canada.
“If students in Quebec are now taking positions outside of Quebec, and students who are hoping to match are not able to, there’s a disparity there,” Moineau says. “The tighter the ratio, the more variables of the playing field, the more challenging it becomes to match.”
“Understanding why Quebec graduates don’t want these positions is key,” Bourgeault says.
To deal with its perceived physician shortage, Quebec has introduced health care reforms, including actions focusing on physician workload, as well as regional medical resource plans that restrict where and how a physician can practice.
A 2014 survey among Quebec medical residents found that 47 percent of those leaving medical residency for professional practice did not have a position two months before finishing their training. Among these residents without a position, 27 percent said they intended to leave Quebec. More than three-quarters of respondents said they believed there were not enough job opportunities for the number of trainees.
Planning for the future
Unmatched Canadian graduates have two choices: they can opt to graduate and spend their time as they choose (perhaps doing a master’s program or research) until the match re-opens the following year, or they can defer graduation and instead take more electives as a medical student.
Neither is ideal, Rizzuti says. “The former automatically puts you into debt repayment as you’re no longer a student. The latter, where they stay another year, means students are paying another full year of tuition. For Ontario, that’s $25,000 to $30,000.”
“Solutions are complex,” Lewis says. “We need to have a better understanding of the types and number of physicians we need in Canada to help inform our students around their career planning and inform educators around curriculum planning. We need to ensure their are adequate residency spots available to our students with consideration of how many undergraduate medical students we should be graduating.”
Moineau co-chairs a national physician resource planning committee that’s currently developing a tool to help forecast future physician needs, which will help make the case for changing student admissions or residency quotas to better align.
“We feel strongly that we need to move to being in a society where we have the right number, mix and distribution to meet societal needs,” Moineau says.
“This is where everybody needs to advocate to government that we need to have appropriate, long-term health human resource plans in place,” Rizzuti says. “There needs to be a broader conversation to be sure there’s proper alignment in all the steps in training.”
Such a call is not new, dating back to at least the mid-1990s, with significant efforts undertaken to do such planning by governments, medical schools and medical associations.
Students may also need more career counselling in the lead up to the match, Moineau says, as disciplines like surgery or laboratory sciences have become segmented, forcing students to choose a sub-specialty, like neurosurgery versus cardiac surgery, which may prove strategically disadvantageous.
Health human resource planners may also need to take a closer look at how provincial funding and politics are influencing graduates’ choices about where to go for residency training.
Training may also need to be revamped to ensure students get exposure to different disciplines, Rizzuti says, as many graduates are still turning away from rural and remote residencies, which could speak to their experience learning in mostly urban medical schools. The interest in family medicine as a first choice has also fluctuated markedly in the last 10 to 20 years.
Opening more training spots for physicians is not the answer, Bourgeault says. In the health system as a whole, there are already a number of health care professionals whose skills are under-utilized, including nurse practitioners, pharmacists, physiotherapists and others.
Instead, medical schools should be thinking about how to attract and prepare the students they need for the positions they’ve got, and continue to adjust the number and mix of residency spots to better meet societal need.
“We need to do that better,” she says. “We have a distribution issue, we don’t necessarily have a numbers issues.”


The comments section is closed.
Remove residents not funded by the provinces( eg Saudis funded by Saudi government )who in essence are using spaces which Canadians could use.
Remove the tight accreditation requirement that all trainees in BC should go through UBC for example. Why has UBC been given such a monopoly? For example in BC Fraser health could run their own program completely and train physicians who would better fill our needs and those trained should have the right to challenge the College of FP exams . What gives UBC the right ? Their training and selection of trainees isnt necessarily the best- clearly they are not training what we need.
Morally, we need to reclassify IMG s into two categories- Canadian born/raised who went to study abroad at their own or their parents’ expense have saved the system money and must be given priority to return to programs in their own country. Secondary are new Canadians .
All trainees should have a return of service requirement if we are going to impose such a thing.
One of the thing to remember is many students from Canada go to UK, Ireland or other European countries because they accept students for med program after High School (Grade 12) whereas in Canada and US you have to complete 3 or 4 years of undergraduate before you can apply for medicine. If residency for IMG is made simpler or equivalent to CMG, then many students will prefer to do their medicine in those countries and come back to Canada for residency and save 3-4 years.
Canadian graduates first, then img! Should not even be considered till all Canadians have a spot. Unmatched students should not have to wait a year . unfilled positions should stay open till they are filled.
I still say Canadian citizens regardless of where they graduate should be considered for placements first, as they will stay and practice in Canada. International students, regardless of where they are taught should be second as they are likely to take their education home…. how does that help Canada beyond the fees paid to the university. It is a broken system at the moment!
My daughter, who graduated from Medical School of America was not matched in the first round in USA. She is Canadian cytizen and I am wondering if she as such has any advantage over international students non Canadian coming from India, Near East or any other country looking for opportunity in Canada. Being Canadian looking for match in USA she was in disadvantage compared to US citizens {ViSA issue}. Does she have also disadvantage in Canada as well, being in the same pot as any other non Canadian graduate. As you know her education cost more than $300,000. She has debt and no job to be able to return that money. How Canada will provide protection to own citizens?
For someone who is a Canadian citizen but is doing medicine in Royal College of Surgeons in Ireland, what are the chances of getting accepted to a residency program in Canada (especially Ontario) ?
Totally depends on your area of focus, Guss
Having the students assessed by pass and fail or making Anatomy elective are simply suminating the medical education in Canada
With respect. the REAL problem for society: ie the medical students AND the public IS the loss of the rotating ” internship” as a path to licensure…students in med 1 are angling their options and learning to a path they can only be minimally aware of… also, consultants have no awareness of, or empathy toward, other physicians, particularly general practitioners…the hubris of the College of Family Physicians of Canada and the demeaning attitude of the specialists toward generalists are the main cause of the problem and are the major impediment to a societal solution…
George Ferrier MD Dal 1973
the fact that quebec had only a few unmatched students, but many unfilled residency positions, shows clearly that few bilingual quebec students want to train in quebec. it is possible that many of the unfilled residency positions in quebec would be of interest to english speaking students from other provinces, but they are not interested in having to contend with the french language requirements. if quebec wishes to attract english speaking students to its residency programs, the french language requirements must be dropped.
4th year med students in Canada write a closing exam. If international students take the same exam then they deserve equal consideration based on the results.
Thank you Howard. Couldn’t agree more!
No they don’t! Have they paid taxes that will cover their salary as a resident? Have they paid university tuition of 150,000 to a Canadian school. I can go on and on! Canadian citizens first, Canadian graduates first
Canadian citizens regardless of where they educate, Mina.
I can see the biased residency match finally is hurting the Canadians as well. I see more and more IMG’s everyday take their distance from getting involved in research and putting time and effort in research for faculties. They are unwilling to participate since they see there is no point bothering. I personally do not bother any more and I know of many as well. Regarding Canadian graduates, well, if you want to see things moving forward, you need to respect your colleagues from other parts of the world as well. Get them involved, increase the spots, get the positions filled. There is still a lot of need in this system but no one bothers to even listen. There should be a balance between working hard and getting accepted. If that balance goes away, everyday you will see that your medical system will go into demise and more talented people will step aside and at the end of the day, the result is what you see today in this article.
That’s the problem here in the USA too. there not the best candidate who gets these positions, are the ones with more connections, if the chairman of a program has specific admiration for specific culture models, guest what: the ethnicity is playing a big roll I know this is not politically correct and nobody wants to speak about, but I’ve seen it myself granting residency spots to certain ethnic group only when the chairman is alined in that direction, and that goes along more with the candidates coming from arab countries, oriental including India, China and all oriental countries; I always asked myself, it’s good to be diversified but never forget that the funding of these programs is by all the citizens of the country
and if the needs of us is not served properly, it’ll only be a matter of time before sudden and severe changes will happen.
John Osky.
These are difficult stories to read but I have one question that I still cannot get a straight answer to. Why are Canadian students who study abroad and who have passed the entrance exams to Canada provided with a fraction of the places on first round picks? The answer I have been given most often is that the Canadian taxpayers have helped to fund students at Canadian medical schools so they must be given first pick to justify the investment. I hope there is a better reason than this because I would hope the best doctors are chosen not the best doctors from an artificial pool. My daughter has studied abroad and has cost the Canadian taxpayer nothing. She has studied at a university that consistently ranks above most Canadian medical schools and yet she is treated as a second class citizen by her home country. I expect someone will point out that she did not get into a Canadian medical school so must be second rate- except we all know that out of many very smart students some will get in and some will not and it’s not always a measure of smartness. I have read that it is not possible to promote Canadian IMG’s above other IMG’s because it might offend the Charter. How does it not offend the Charter to deny Canadian citizens who have demonstrated their fitness to practice- equal opportunity to compete in first round picks? As a taxpayer myself I repeat that I would hope we hire the best doctors (which may or not may not be my daughter) and not the best doctors from only those who graduate from Canadian universities.
This is a very controversial topic. We’ve written a bit more about the process for IMGs here: http://healthydebate.ca/2014/06/topic/international-medical-graduates-canada
Thank you for your reply. I had read that piece and this is the part I cannot get past:
Over 90 per cent of Canadians studying abroad hope to return to Canada for their postgraduate training, and some people have even called for their preferential treatment over other IMGs. But that may be a violation of the Charter of Rights and Freedoms, since the Canadians would be getting ahead just because of their country of birth.
For me the wrong question is being asked. Why are Canadian citizens not given the same opportunities as their fellow citizens who trained at Canadian schools? Why is that not a Charter infringement? Once it is established that a Canadian trained abroad has the required qualifications, they should be treated equally with any other Canadian citizen. The way the system works now encourages an elitist attitude amongst those at Canadian schools and restricts the pool of available expertise. Why do we not have a policy of hiring the best doctors from among all of our citizens rather than giving an unfair advantage to those trained in Canada? Can you tell me who makes these rules?
So you’re suggesting that all IMGs, Canadian-born and otherwise, should compete equally with those who went to Canadian medical schools?
Seems to me there is a significant immigration hurdle for non-Canadians which may practically restrict the applications to mostly Canadian citizens anyway (there is no constitutional reason why we can’t regulate the immigration of persons seeking scarce medical positions that can be filled by Canadians) but sure, in theory, it shouldn’t matter where the training was received if it is a creditable institution. If someone is the best candidate for the position then he/she is the best candidate. To have a policy which artificially excludes someone graduating top of their class at Harvard in order to make a place for the person who graduated bottom of their class at, say, University of Saskatchewan is indefensible. Don’t we want the best doctors we can possibly attract?
I believe immigration is a separate issue – which is why it may be unconstitutional to differentiate between Canadians who were born here and Canadians born elsewhere. Another argument often brought up is that we’re paying for medical school, so we don’t want to invest in that without getting results from that money. I do feel for the IMGs, though. I’m not sure what the answer is.
The argument that we are paying for Canadian graduates is, with respect, flimsy at best. How does this guarantee we are getting the best doctors? Would we really discriminate against students from world class medical schools? Distinguishing (or discriminating) on the basis of citizenship would seem to me to be justified and reasonable – distinguishing between Canadian citizens on the basis of where a person studies is indefensible.
No. I’m saying that all Canadian citizens who demonstrate competency to Canadian standards should have equal opportunity to compete. I can see no justification for giving only those who go to Canadian medical schools the greatest opportunity.
Do you know who puts this rule in place?
Why do Canadians go to foreign medical schools in the first place.?
If they qualify why go to the extra expense?
Because they CAN’T get in! My son was on the Deans list at Dal and couldn’t get in, so is in Trinity College Dublin and applied to restart just to get into McMaster so he could do his rotations, internship and practice here in Canada… and they turned him down.. didn’t even ask for an interview because “ he was already in med school somewhere!’
Canadian citizens.. regardless of where they educate, if they do well on their exams. Should be considered for placements FIRST! To keep the education in CANADA! Why are we educating foreign students to take that knowledge elsewhere when we have a shortage of physicians here!!!!!!
Love your comment Lynn and completely agree.
I am so sorry to read the story of your boyfriend as a victim of the matching process. I had no idea that this is happening in medicine today since 2009. It is akin to the law schools cranking out law students knowing 25% of them will not ever find an articling position.
Common sense using the data presented in this article seems to indicate the following as a solution options…
1. Asking all potential medical students in the future to be fluent in the French language
2. The majority of unmatched positions are in Quebec on account of the language requirements. The majority of the unmatched candidates are English speaking. It is a “no brainer” that the other provinces needs to provide more training spots… I beg to differ from one of the comments “Of course, the solution is not to provide more funding for the training of residents” … What!
It is exactly what this issue requires as a solution…A) an equal number of positions to the number of all candidates (both IMG and Canadian graduates. and B) Funding that is “flexible” in terms of designation within a large institution. Thus, if there is an unmatched position in Internal Medicine within a funding jurisdiction, that funding can be applied for by the traditional department where there is a lack of practitioners such as family medicine, emergency medicine where it is logistically easier to accommodate an additional resident than a surgical subspecialty.
There is a solution to this terrible situation and it will require the cooperation of all provinces to work together rather than the ” old fashioned approach…That is not how we do it in our province!!!!” This is the preamble statement to failure.
I have just retired from Emergency Medicine after a 44 year career and am still working in the community as a WIC MD trying to help those who are without doctors. It is interesting that we are talking about young MDs who wants to work and can’t find a job or a match. Yet the CIHI data from last year indicated the average male GP worked 0.89 of a FTE and the average female GP MD worked 0.69 of a FTE. How does that fit into our discussion? It indicates the people in charge of supply and demand of MDs who should know just don’t know. There has to be a revamp of this system with leadership based on common sense and not based on politics, jurisdiction or tradition.
Charles
I am an unemployed Canadian specialist. I want to retrain but cannot due to the restrictions on residency positions and access to them. It is getting worse for everyone now.
I take issue with the following statement:
“On an individual level, although being unmatched is stressful and a loss of a year, historically, virtually all unmatched students find success in subsequent years.”
Let’s cool it with the rosy language.
Matching out of desperation is not success. It’s settling.
Going into psych because you couldn’t get a spot in ENT is not success. It’s desperation.
Call it what it is.
Hi Sandy,
Sorry to hear about your boyfriend. I would suggest he apply to the States as well because they have a lot more spots than here in Canada. This year he should concentrate on writing the usmle and getting good scores on it. I wish him the best of luck in the future.
continued…
I am proud to date my boyfriend as he is a wonderful, kind human that attempted to dedicate his life to helping others but others won’t give him a chance to prove he is worthy of a spot. He is the bravest, smartest, most hardest working person I know and for that he makes me proud. He has made me more hardworking, more dedicated, smarter, more skilled, etc and for that I am darn lucky.
If any of you doctors or program directors have any advice please respond! Help is welcome and would be greatly appreciated.
Holy! That’s unbelievable. Definitely the worst CaRMS story I have ever heard. I’m so sorry. I hope someone more useful than myself can respond to this…
Yeah, someone give this guy a spot, seems like he’d make a decent doctor.
Dear Sandy,
Thanks for your story. I appreciate your openness and sincerity. Sadly, I cannot offer you any advice/help from a program directorship or academic viewpoint as I work in rural area. From what you have written, this physician demonstrates a passion for the science, determination and tremendous work ethic, and I can affirm that these are qualities essential to a rewarding medical practice. My limited seven year teaching experience of students and surgical residents has given me appreciation for those who are versatile, innovative and flexible, as this doctor has endeavoured to be. I can relate, in some respects, to your situation as I am in a field where surgical employment was limited and I know what it feels like to have no work after all the training. The experience was difficult but gave me a reality check to truly appreciate the privilege we are awarded to care for the sick, no matter in what route that ultimately transpires. I want to thank this colleague for his hard work, and that he recognizes the accomplishments he has already achieved. I do hope that he does someday achieve his desired objectives. Although a matching process is very stressful, I hope that you are able to help each other navigate the important things in life, remain steadfast from the distractions of unprofessional behaviour, and continue to deliver the best service possible in the care of your patients. Best wishes!
Hello Sandy,
I am ex rural GP and soon to be retied surgeon. My wife and I are from the era before the match and have three children who went through match stress ( two in the highest demand ). I really feel we should match all our students. I also think there should be more lateral movement between disciplines ( 40 to 60 years ago about 20 % of specialists were retreads like me ), In your situation your diligent boyfriend needs a mentor that can go to bat for him not just paperwork. I hope it works out.
Ian,
I agree with you completely.I too am an ex-rural GP (briefly, one terrific year) from the pre-match era. The university surgical program effectively gave me that year as a sabbatical.
I was prepared (adequately, I thought) , by 4 intensive med school years and one super-intensive rotating internship year at a large Canadian teaching hospital.
Were does it say that family medicine requires more? We did have the Krebs cycle, labs, X-rays, antibiotics, EKGs even then. And meaningful, hands-on rotations in EVERY discipline….IM, general surgery, OB-GYN, psychiatry, ER medicine, and various sub-specialties.
So (then) , I could do what I saw my own family doctor did on his house calls and in his practice. And , while valuing that experience, knowing that specialization was what I wanted, I delivered babies, did tonsillectomies, house calls, surgical assists, and ER medicine. And felt qualified to do so. And loved it.
I then started in a premier general surgery program , and switched to orthopedics at the same premier university program, (my choice…. ortho program invited me). I could have finished general surgery but lateral-shifted to the specialty that found me and I it. Possible then! Better for me and for general surgery, probably.
I retired 41 years later after a great experience in orthopedic surgery practice.
My daughter-in-law, an A-student graduate in a Canadian medical school,was, recently not even given an interview in family practice anywhere in Canada.
She then matched in internal medicine (not her first or best choice) and will , with two children and husband , finish more years later, possibly uprooting her family and career-path “tenured” husband, to another province after 10+ years where they are. Such injustices abound, it seems.
How can this present system in any way be fair to these young people who have invested so much, in their time, toil and money?
My relatives fight to find and keep primary care MDs, then to get timely referrals to specialists.
In what universe does this present system work for anyone, doctor or patient?
Sandy’s and many others’ matching horror stories break my heart and are poignant examples of a broken , inhumane and inefficient system, with suspect parameters. And ,in this greatest ,noblest profession, to not be able to go forward is sad, and bad for the profession and its patients.
So, Sandy and Ian, I agree. Everyone should match on graduation and lateral movement between disciplines is desirable.
Your boyfriend should try applying to anesthesiology in the USA. They have more spots and provided he scores well enough on the board exams, he should be able to get a spot somewhere. He should then proceed to stay in the USA to practice indefinitely. Canada doesn’t deserve him.
Hi Sandy, do you have an update on your boyfriends situation? I am a new medical student and his story is frightening beyond words. Thanks.
Dear Sandy,
This is an extremely difficult situation. I can only imagine how he feels. He is obviously resilient and must not give up. I would suggest that he applies for residency in the US since 50% of IMG are matched.
It is defenitely unfair that an IMG would be matched before those who did residency in Canada[ I am not a Canadian].
It is saddening, the lack of empathy and the immaturity displayed by your coworker. But bullying is not a reflection of you or your boyfriend, but I feel, about that person’s own insecurities, and the need to put another person down to feel good about themself. I believe that you should politely tell that person to stop with their comments. Who wants to be dealing with bullies on a dad to day basis.
continued…
any patients, not interested in looking at any lab values, she was only interested in asking the nurse a bunch of questions so she would get the answers without rounding or looking up lab values. Things were so bad that I told my mother who recommended next time in the same situation to just go hide in the bathroom. Yet, this resident then further matched to a popular pediatric subspecialty. I had the opportunity to work with 1 3rd year psychiatric resident who was constantly forgetting form expiry dates, frequently letting forms lapse accidently, discharging patient’s while certified under the mental health act, ordering labs and blood work under the wrong patient. He blamed the nurses for not notifying him about the forms when the charts were made available to him, form statuses was written for every patient on a white board in the nursing station and in the daily assignment binder in the nursing station. To see all these people get a chance and then not to see boyfriend get a single chance breaks my heart.
Due to CaRMS and my boyfriend not matching we have had defer getting engaged, getting married, having children. We both still live at home as it makes no sense to settle into a home for a short time if he were to match in the future. because we would most likely have to move. It is hard to make a solid plan for the future if your future may be on the move. My boyfriend tries year after year for CaRMS. Every year I hope and pray this will be the year and the last time we go through this.
CARMS is a huge source of my stress, relationship problems, it has caused unhappiness and the ability to plan for any type of a future. I have spent countless hours helping with ideas for impact statements, ideas for interview questions, videos other students made while going through CaRMS. I have dedicated time to help him on my days off, while on vacation yet nothing ever seems to help. The amount of hours have spent crying, all the sleepless nights, all the days I felt sick sick/ nervous with stress and fear to eat, all the days I was a shitty person or nurse due to the stress of CARMS, all the relationship arguments, putting my life and my kids on hold, hoping for a better future…… I would never wish what I have gone through with my boyfriend with even my worse enemy. No one deserves to be dragged through Hell and back the way CaRMS has to my boyfriend. U of T medical school does not even care. They won’t even help him for one second. Yet, U of T has a history of handing out spots outside of CaRMS. This is not allowed but yet schools do it e.g. when a participant drops out of their program which is not suppose to happen then the spot just gets handed to some one a silver platter and a get a residency they never matched to. Some people get lucky while others have terrible luck. Everyone deserves a chance.
They should only make enough medical school spots as there are residencies.
care to those in need. He hopes to include the care of elderly in my practice. He chose Anatomical Pathology to help me better understand sample analysis.This is important as I may have potential patients with lumps, bumps, masses, moles that may need sampling and biopsies. He chose Emergency Medicine to help him practice certain skills that are applicable in family practice eg. Suturing. He also hoped to gain skills, practice, knowledge and confidence should an emergency arise while practicing family medicine. In January 2017, he returned to Humber River Hospital to participate in the teaching and delivery of a 2 day course that focused on ultrasound as a diagnostic tool in the ER.
He participated in CaRMS in 2017. Despite recently completing all these electives (more electives that current medical school graduates), having done post graduate research and publications, doing the post Grad MD program he did not get a single interview despite applying to many programs. Post Grad MD was an additional $8,000.00. He was unmatched for a 3rd year.
It breaks my heart to go to work and work with 1 particular co-worker. I have 1 friend that I work with whose husband got U of T internal med for a residency. He went to undergrad at U of T, did not apply to medical school in Canada (most likely his grades were to low) and he went to medical school in Ireland (University College Cork School of Medicine). Her husband was one of the lucky 421 IMGs to match. She always talks about how he deserved a spot, how hard he worked during medical school, how they had to have a long distance relationship where they could not talk everyday because he was so busy working with medical school. She is constantly making fun of me and bullying me in the workplace. She always tells me I don’t date a real doctor, and he must have not worked hard, we should just break up and how much of a loser I date because he did not get a residency. But her husband could not get into a Canadian medical school but yet got a residency at U of T. Do any of you know how that feels (to go to work on a daily bases and be told to break up with the person you love because he must be a loser for not getting a spot)? I am bullied on a daily bases for dating some one that was left without a residency. Do any of you know how humiliating that is to be bullied in the nursing station and have the person you love most to be called a loser in front of everyone. I know how hard my boyfriend worked, how smart he is and how he got robbed of a spot. When doctor’s day 2017 came up on May 1/17. I made my boyfriend a card to help him celebrate all he has achieved. My friend told me he is not worthy of a card because he is not a real doctor despite earning an MD from U of T.
It breaks my heart to see other medical students and residents be given a chance but no one will take a chance on my boyfriend. It has tore my heart out of my body to see ill prepared medical students show up for placement not even knowing how to write progress notes following their examination of a patient and then they match. I have seen 1 3rd year pediatric resident show up for placement without a clue how to read an ECG, not interested in seeing
continued…
Following medical school graduation he worked on research projects and publications with world renowned Dr. David Jenkins and his medical team at St. Michael’s hospital in downtown Toronto, Ontario. After months of research projects he decided to return to U of T to complete courses in Computer Science. After completing a total of 8 4th year courses he would be able to add a major on to his existing degree. In no way was he quitting or giving up on medicine. He was interest in perusing education that could compliment both his skills as a MD and would be useful as medicine is continuously evolving from paper to the electronic form. Both computer technology and E health are becoming a way of the future. For example: Hospital, clinics and practices are converting paper physician orders, physician notes, allied notes, charting, medication administration records to the electronic forms. Mental health act forms are now being scanned into electronic documents. CPS manuals are only available in electronic forms. By being knowledgeable regarding computer programming and software he would be able to keep current with the latest medical charting and health care systems, keep up with current health care models, are able to lend support/ aid to various physician offices, clinics, hospitals that are in the process of converting from paper to the electronic form, are able to encourage physician offices, clinics, hospitals that are on paper to convert to the electronic forms and then lend support in the process of change and ae able to also look at computer related issues as they arise. For example: a malfunctioning computer in private practices or clinics may not always have IT support. While perusing his interest of computers which will ultimately help him in his practice as a physician I was still involved in medicine. For example: he took CPR, took ACLS, completed an observer ship in radiology at The Brantford General Hospital, was involved in my father’s family medicine practice , read medical journals, etc. He hoped to increase his knowledge of reading and interpretation x-rays, ultrasound results and other diagnostic tests.
He sat out both interations of CARMS in 2015 as he was working diligently to earn a major in computer science that he thought could complement him later in his medical career. He also worked part time in computers to help pay back his medical school debt.
In 2016, he applied to 50 family medicine programs across 6 medical schools. He was left with one interview. He did not match in the first iteration. He applied to family medicine and anesthesiology (over 20 programs). He had 3 interviews and was unmatched yet again.
In August of 2016 to December 2016 he returned to U of T medical school and enrolled in more electives (Post Grad MD) to increase his ability to match. During this program he focused on family medicine, rural family medicine and other specialties that can strengthen his knowledge and skills as a physician that can be used in family medicine. He completed 2 weeks of family medicine in an office on the East Side of Toronto, a 1 day observership in Palliative Care at Brampton Civic Hospital, 3 weeks of Anatomical Pathology at Trillium Health Partners, 4 weeks of rural family medicine at Guelph Practice (with The Rural Ontario Medicine Program) and a little over 2 weeks- Emergency Medicine at Humber River Hospital (North America’s first fully digital hospital). He hoped Palliative Care would teach him how help provide compassionate
My CaRMS Story
In March of 2013 I met my best friend and now boyfriend. I was working as a nurse at Toronto hospital when I met a lovely young man in was in his third year of U of T medical school. We quickly became friends and were good friends for 2 years before we started dating. His solid worth ethic, rounding early, great note making, knowledge and ability to answer physician’s questions really impressed me. He inspired me to work hard and become a better nurse.
He did mathematics and sciences at U of T for undergrad. He was on scholarship every year. He had final multiple grades of 100% in undergrad courses. One of his 100% was in statistics. He wrote the MCATs once and scored nearly perfect. He applied to medical school right after undergrad. He had multiple medical school interviews in Ontario and accepted an offer to attend U of T medical school.
Prior to going to medical school he thought he would be guaranteed a residency following the completion of medical school. Never in his wildest dreams did he think he would face the problems he has faced (not matching). Going into medical school he had wanted to do family medicine as his father is a U of T medical grad is an amazing family physician. After exposure to different specialties after third year of medical school he was unsure which discipline would suit him best. He sought guidance from faculty at U of T medical school. They recommended anesthesiology. In 4th year he did a ton of anesthesia research and every elective was in anesthesia. He did rotations all over Canada. He packed himself up, left his car behind, his 7 siblings behind (one of which was 7 at the time), the rest of his loved ones behind and travelled to other provinces to complete anesthesiology electives. He had no family, no friends in these other provinces, lived out of a suit case, lived out of hotels, etc. He did this to help give him a great chance to match. His hope would be to match anywhere in Canada for anesthesiology. His 4 year U of T medical school costs were $125,000.00
March 5, 2014 came where he learned he did not match in the first iteration despite having 9 anesthesiology interviews across the country. When the unfilled spots came out Ottawa anesthesiology had 1 spot unfilled and Ottawa was not one of the 9 schools that had offered him an interview. Not only did he have to deal with the fact he was unmatched but he was also blamed by his ex girlfriend as the result of her not matching to her top choice (U of T internal medicine). She did match to U of T family medicine- rural program. This seemed hardly fair when he got left with nothing. But he did not give up and applied in the second iteration. He had interviews in radiology and family medicine. He had done 4th year selective in family medicine, internal medicine, etc. Once again he went unmatched. He then wrote the MCCQE part 1 and did very well.
This is my opinion as a program director. I would propose limiting applications to 5..most students match in their top 3. Then have a 2nd iteration for only unmatched students..again limiting applications to five. Keep doing this until everyone is matched. In other words..all students who graduate have the option to match…or to withdraw which is their choice. Next would be an IMG match. The numbers we currently get are unwieldy and make it very difficult to identify those who most want us…so most lose out when in fact they might not if we knew they were the top 5 choices.
I’m a current resident and completely agree. It’s so senseless travelling the entire of Canada to numerous interviews when either one or both parties are not seriously considering the other. It costs about 3000 dollars and it’s a lack of respect for the financial stress students are under.
I didn’t read the full article because the pain is bad right now, but for God’s sakes match these students so that we don’t have doctor shortages anymore. People in some Northern Ontario (North Bay, in particular) cities are desperate for family physicians and specialists. The one clinic that is accepting patients in North Bay, Ontario requires that patients fill out a detailed application and once the application is completed, there is a one year waiting list for a meet and greet appointment and the clinic may not even accept you as a patient after the meet and greet appointment.
The problem is that moving forward, there’s going to be a bottleneck effect at the level of the residency match. Why are medical schools continuing to maintain enrolment numbers and at certain schools, increasing enrolment in light of this? Medical schools need to decrease enrolment or the government must find better incentives for graduates to practice in underserviced areas.
Ontario stopped having two separate pools (blending IMG and CMG into one stream) in the second iteration in 2009, the same year the unmatched CMG numbers started to increase. Perhaps the provinces should look at “un-blending” the second iteration and possibly leaving just the unfilled IMG positions as blended. This may help in addressing the unmatched CMG issue. This change can be easily made and un-done (in future matches) if it proves to be not improving the number of unmatched CMG’s.
One correction to the above, the first iteration is open to both newly graduated CMG’s and CMG’s who went unmatched in previous years (provided they do not have any postgraduate training).
As the Mom of a son who couldn’t get into medical schools in Ontario but was immediately accepted into a very prestigious school in Dublin, Ireland.. I blame the number of International students getting into Ontario Med schools in the first place (for the sake of the increased revenue for the school!) To think he won’t even have a chance for a first round placement in his own province is heartbreaking. This system in clearly broken. Specially when it’s clear those foreign students will likely be taking their knowledge home with them at the end of it all!
Ontario med schools require students to be Canadian citizens or permanent residents. They may be immigrants but it’s almost certain their intention is to practice in Canada.
As an IMG and a PR holder I find it outrageous that for every unmatched Canadian into the residency or a failure to get into the medical school, someone has to blame the international students. Do you know the amount of requirements we need to go through so that we are legible to apply for the exams and at the end we still don’t get matching seats? We are leaving everything behind, we are exposed to enormous amounts of expenses, we are as qualified as the Canadian students and we are still being blamed for every failure of yours.
One point I wish I had made more clearly in the article isnthat whatever the cause the impact on the individual can be really upsetting for many of them. Let’s all be sympathetic and supportive to our colleagues
Speaking as someone who went through this last year, I can say that it is very upsetting. You feel alone, confused and no one can give you answers. I interviewed at 10 out of 11 programs for a mid-competitive specialty, had 9 publications and great feedback at all my rotations etc. etc. Typical applicant with strong research background.
I’m happy to say that I’m thrilled at where I matched this year, and I had an extremely introspective year, but the number of students who completely flounder after going unmatched is too high.
I agree that we need to:
(a) Train fewer medical students if residency spots are going to be cut… *cough* I’m alluding to the 50 that Wynne cut over the last few years in Ontario*.
(b) QC needs to start treating their doctors better! That 27% might not want to leave if they did!
(c) As an Ontarian, the bickering OMA vs. Government really has skewed people away from Family Medicine. Students were concerned that a future in family medicine is worrisome so they applied to Internal instead. Made the Internal match uber-competitive this year.
Hi BJ
Congrats on matching. Sorry to hear your struggles and I am glad you did not give up. All the best in your future career as a doctor!
I was an unmatched loser ten years ago. Took what I could get in the loser round. Hate it still. Seeing what happened to Sandy’s boyfriend is sickening and could have been my fate had I not licked the crumbs from the side of the table like a good dog, after all of my betters got the choice picks. I could have been starving. It’s better to practice medicine in something I loathe than to not practice at all. That’s what I tell myself. But it is hard to look myself in the mirror and see success and worth. I just see a loser. That’s where the chips fell, and there’s no climbing out of that sewer, as Sandy’s boyfriend’s experience shows us all. The system knows all, we are merely parts of it.
The worst part is you never know why. Why you’re so much worse than everyone else. You can’t fix it because you don’t know where you’ve gone wrong. In my case I looked at everything: my reference letters, my dean’s letter, my elective evaluations, everything. There were no red flags, no hiccups, no “hidden meanings” between the lines. What else could it be? Is it me? Am I that bad?
Sandy’s boyfriend deserves a position. He worked hard and showed his determination. The way the system is set up is that if you don’t get a position the first time, you’re obviously a LOSER and shouldn’t have gotten into medical school in the first place. I think most of the people who have read Sandy’s boyfriend’s article here are secretly thinking to themselves “there must be something wrong with him, which is why nobody wanted him”. It is not fair.
A med student at Mac killed himself after not matching twice for no good reason, even after he lowered his sights and applied broadly. It’s bad enough when they field you’d like to practice in considers you worse than filth, but all other fields? That’s brutal. I get why he did it. People are going to attribute it to the broad stroke of “mental illness” but – and I’m not condoning suicide in any way – I argue it was a rational decision on his part. Not matching is a huge public shaming. You’re exposed to your peers and your superiors as being “unworthy”. It’s human nature, written about by Shakespeare and others, to want to exit life when you’ve been so humiliated and flayed, without any recourse or hope for redemption.
Matching system is done by algorithm, running on multiple classifications. And current knowledge shows, that humans outperform computers in solving for conflicting and competing classifications. The bias set into first choice rankings based on empiric assumptions of perfect match. There is no names, accountability or any repair to fix the inflicted harm of wrong match or absence of any at all. What about the personal opinion of the preceptors? How much that component weights? Not known.
Putting back Humanity in Medicine is important not only for Patients and their families, but for physicians first. Seeing ourselves with dignity and respect is setting up the field.